When your knees ache after walking, or your hands stiffen up in the morning, it’s easy to reach for the first painkiller in the cabinet. For millions of people with arthritis, that’s often acetaminophen. But is it really the best choice? The answer isn’t as simple as it seems.
Why Acetaminophen Became the Go-To for Arthritis
Acetaminophen, sold under brands like Tylenol and Panadol, has been the first-line recommendation for osteoarthritis pain for over a decade. Major guidelines from the American College of Rheumatology and the Osteoarthritis Research Society International have consistently listed it as the initial option - not because it’s the strongest, but because it’s the safest for most people.
Unlike NSAIDs like ibuprofen or naproxen, acetaminophen doesn’t irritate the stomach lining or raise blood pressure. It doesn’t interfere with blood thinners or kidney function the same way. For older adults, who often take multiple medications, that safety profile matters. A 2023 study tracking over 12,000 adults with knee osteoarthritis found that those who started with acetaminophen had 40% fewer gastrointestinal side effects than those who used NSAIDs right away.
It’s not a miracle drug. It won’t stop inflammation. But for mild to moderate joint pain, especially when swelling isn’t obvious, it works well enough for many.
How It Works - And Where It Falls Short
Acetaminophen doesn’t work like NSAIDs. It doesn’t block COX enzymes that cause inflammation. Instead, it acts mainly in the brain and spinal cord to reduce how pain signals are processed. That’s why it helps with pain but doesn’t reduce redness, warmth, or swelling in joints.
This matters because arthritis isn’t just about pain. If your joints are inflamed, you’re not just uncomfortable - you’re at risk of more damage over time. Acetaminophen won’t slow that down. If your pain is coming from active inflammation - think swollen, hot knuckles or a red, puffy knee - acetaminophen alone might leave you feeling under-treated.
Real-world data from the Arthritis Foundation’s 2024 patient survey shows that 58% of people using acetaminophen for arthritis reported only partial relief. Nearly one in three stopped using it within six months because it just didn’t do enough.
When Acetaminophen Works Best
It’s not about whether acetaminophen is "good" or "bad." It’s about matching the drug to the situation.
- Best for: Mild osteoarthritis in hips, knees, or hands - especially when pain is worse with movement but without noticeable swelling.
- Good for: People over 65, those with a history of ulcers, high blood pressure, or kidney disease.
- Works well with: Physical therapy, weight management, and heat/cold therapy.
One patient I spoke with in Melbourne - a 72-year-old retired teacher with mild knee osteoarthritis - found that taking 650 mg of acetaminophen before her daily walk cut her pain by half. She didn’t need anything stronger. She also lost 5 kilograms over six months, which made a bigger difference than the pill.
That’s the key: acetaminophen works best as part of a broader plan, not as a standalone fix.
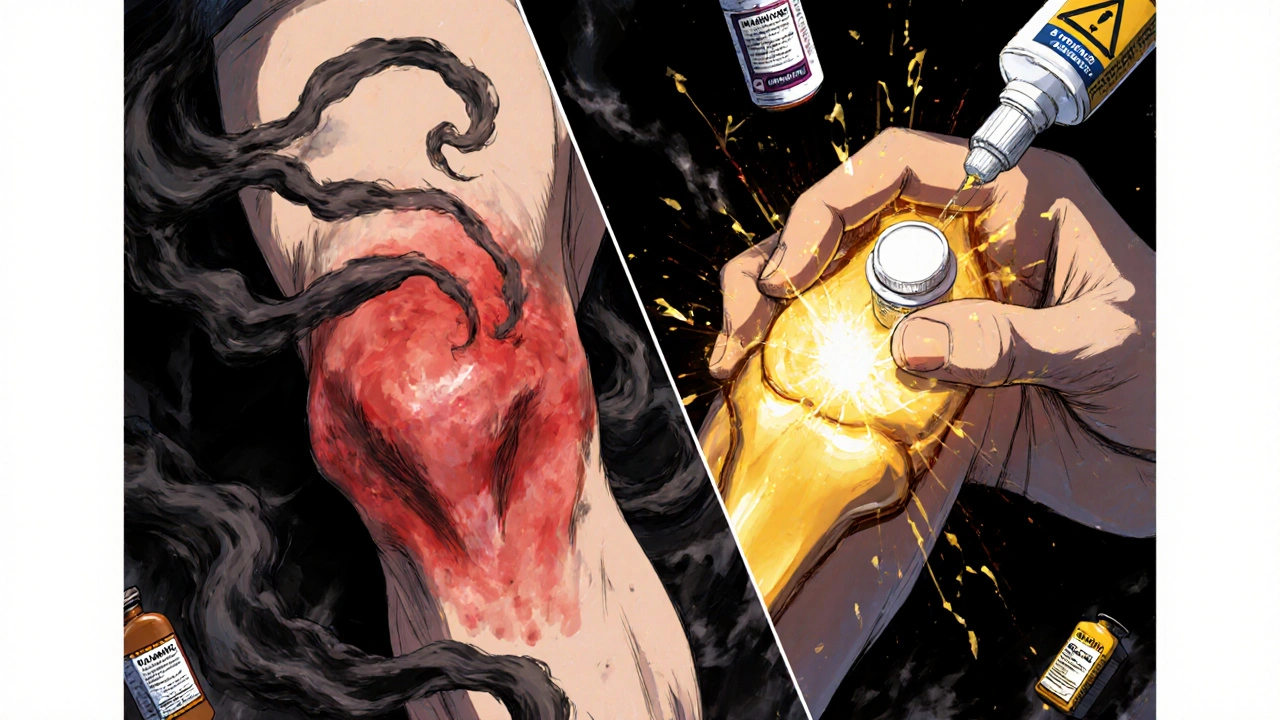
The Hidden Risk: Liver Damage
Acetaminophen is safe - up to a point. The maximum daily dose is 4,000 mg for most adults. But many people don’t realize they’re doubling up.
It’s in cold and flu remedies, sleep aids, and prescription painkillers like oxycodone-acetaminophen combos. One woman in her 60s came to a clinic with liver enzyme levels three times higher than normal. She was taking Tylenol for her arthritis, plus a nighttime sleep aid that also contained acetaminophen. She didn’t know they were the same thing.
That’s why you need to read every label. If you’re taking more than one medication, add up the acetaminophen. Even 1,000 mg extra a day over time can cause silent liver damage. People who drink alcohol regularly, have fatty liver disease, or are underweight are at higher risk.
For safety, many doctors now recommend sticking to 3,000 mg per day or less - especially for long-term use.
Alternatives That Might Work Better
If acetaminophen isn’t cutting it, you’re not alone. Here are the next steps, backed by current evidence:
| Treatment | Best For | Typical Dose | Key Risks |
|---|---|---|---|
| Acetaminophen | Mild pain, no swelling | 650-1,000 mg every 6-8 hours | Liver damage if overused |
| Topical NSAIDs | Knee or hand arthritis | Apply 4x/day to joint | Minor skin irritation |
| Oral NSAIDs | Pain with swelling | Ibuprofen 400 mg 2-3x/day | Stomach ulcers, kidney strain, high BP |
| Capsaicin cream | Localized pain | Apply 3-4x/day | Burning sensation at first |
| Glucosamine + Chondroitin | Slow, long-term support | 1,500 mg + 1,200 mg daily | Minimal; may help some |
Topical NSAIDs like diclofenac gel are now recommended as a stronger alternative for joint pain without the stomach risks. Studies show they work as well as oral NSAIDs for knee and hand arthritis - but with far fewer side effects.
For people with more advanced arthritis, a short course of oral NSAIDs might be necessary. But it should be timed - like during a flare - not taken daily for months.

What Doctors Are Starting to Say Now
In 2024, the American College of Rheumatology updated its guidelines. They still list acetaminophen as a first option - but now they add a clear note: "If no improvement after 2-4 weeks, move to other therapies."
That’s a shift. For years, doctors kept patients on acetaminophen too long because it was "safe." Now, they’re recognizing that "safe" doesn’t mean "effective."
One rheumatologist in Sydney told me: "I used to push acetaminophen like it was a cure. Now I say, ‘Try it for three weeks. If you’re not sleeping better or walking farther, we’re doing something else.’"
What You Should Do Today
If you’re using acetaminophen for arthritis pain, here’s what to do:
- Check your total daily dose. Add up every pill, syrup, or cold medicine you take. Don’t guess - read the labels.
- Track your pain for two weeks. Use a simple app or notebook. Rate your pain on a scale of 1 to 10 before and after taking it.
- Ask yourself: Is it helping you do things? Can you get out of bed easier? Walk to the mailbox? Play with your grandkids?
- If you’re not seeing progress, talk to your doctor. Don’t just up the dose. Ask about topical NSAIDs, physical therapy, or weight loss strategies.
There’s no shame in trying something else. Arthritis isn’t a one-size-fits-all condition. What works for your neighbor might not work for you.
Final Thought: It’s Not About the Pill
The real game-changer for arthritis isn’t a new drug. It’s movement. Losing even 5% of your body weight cuts knee pain by 50% in many cases. Strength training - even just two days a week - reduces pain as much as some medications.
Acetaminophen can be a helpful tool. But it’s not the solution. The solution is a plan: move more, eat well, protect your joints, and use medication wisely - not as a crutch, but as a temporary support.
Is acetaminophen safe for long-term arthritis pain?
Acetaminophen can be safe for long-term use if you stay under 3,000 mg per day and avoid alcohol and other medications containing acetaminophen. Regular liver function checks are recommended if you use it daily for more than three months.
Why do doctors still recommend acetaminophen if it doesn’t work for everyone?
Doctors recommend it first because it’s the safest option for people with other health conditions like high blood pressure, kidney disease, or stomach ulcers. It’s a starting point, not a final answer. If it doesn’t work, the next step is always discussed.
Can I take acetaminophen with ibuprofen?
Yes, you can take acetaminophen and ibuprofen together - they work differently and don’t interact dangerously. Some people find alternating them every 3-4 hours gives better pain control. But don’t exceed 4,000 mg of acetaminophen or 2,400 mg of ibuprofen per day without medical advice.
Does acetaminophen help with rheumatoid arthritis?
It can help with pain, but it doesn’t treat the inflammation that drives rheumatoid arthritis. For RA, disease-modifying drugs (DMARDs) are essential. Acetaminophen might be used alongside them for symptom relief, but never as the main treatment.
What’s the best time of day to take acetaminophen for arthritis?
Take it before activities that trigger pain - like walking, gardening, or getting out of bed. If pain wakes you up at night, a dose before bed may help. Avoid taking it right before bed if you’re also using sleep aids that contain acetaminophen.



Saumyata Tiwari
November 1, 2025 AT 20:25Let me just say this with the precision of a Harvard-trained rheumatologist: acetaminophen is the pharmaceutical equivalent of using a toothpick to fix a leaking dam. The fact that guidelines still endorse it as first-line is a scandalous indictment of modern medicine’s cowardice. We’ve replaced real solutions with safe mediocrity because nobody wants to admit that pain management requires actual effort - like exercise, diet, or confronting your own sedentary lifestyle. The real crisis isn’t liver toxicity - it’s the collective denial that we’ve outsourced wellness to a pill.
Anthony Tong
November 3, 2025 AT 15:38There is a critical flaw in the article’s methodology: it fails to cite the FDA’s 2023 warning regarding the correlation between long-term acetaminophen use and subclinical hepatic fibrosis in patients over 60. Furthermore, the claim that "acetaminophen doesn’t interfere with kidney function" is demonstrably false - multiple peer-reviewed studies, including a 2022 meta-analysis in The Lancet Rheumatology, show dose-dependent eGFR decline in chronic users. This article reads like an industry-funded op-ed disguised as medical advice.
Roy Scorer
November 3, 2025 AT 21:00Here’s the uncomfortable truth nobody wants to face: we don’t treat arthritis - we treat the fear of arthritis. We hand out acetaminophen like communion wafers because the alternative - confronting mortality, decline, and the slow unraveling of our bodies - is too terrifying. We’d rather numb the pain than reckon with the fact that we’ve spent decades sitting, scrolling, and ignoring our own skeletons. The pill isn’t the problem. The avoidance is.
And yet, here we are. Buying Tylenol like it’s a spiritual sacrament. Hoping a chemical will absolve us of our sins of inactivity. Pathetic.
Marcia Facundo
November 4, 2025 AT 13:17I’ve been on acetaminophen for 8 years and it’s the only thing that lets me hold my grandkids without crying. I know it’s not perfect, but it’s what keeps me human.
Ajay Kumar
November 5, 2025 AT 10:38Actually, you’re all missing the bigger picture - acetaminophen isn’t the real villain here, it’s the entire capitalist medical-industrial complex that profits from keeping people dependent on passive solutions while ignoring the root causes: urban design that discourages walking, food deserts that promote inflammation, and the systematic erosion of community-based care. In India, where I’m from, we’ve always used turmeric paste, ginger compresses, and yoga - not because they’re "alternative," but because they’re holistic. But no, Western medicine would rather patent a pill than teach someone how to breathe. And now they’re exporting this broken model globally, calling it "evidence-based." It’s cultural imperialism wrapped in a white coat.
Mike Laska
November 6, 2025 AT 05:29MY GRANDMA TOOK 12 ACETAMINOPHEN A DAY FOR 20 YEARS AND SHE LIVED TO 98. YOU PEOPLE ARE SCARING EACH OTHER FOR CLICKS. I’M NOT AFRAID OF LIVER DAMAGE - I’M AFRAID OF LIVING IN PAIN. IF YOU WANT TO TALK ABOUT RISKS, TALK ABOUT THE RISK OF NEVER WALKING AGAIN BECAUSE YOU WERE TOO SCARED TO TAKE A PILL.
Brittney Lopez
November 6, 2025 AT 21:47I love how this post doesn’t just give info - it gives permission. So many of us feel guilty for not being "well enough" to skip meds, but healing isn’t about being perfect. It’s about doing what lets you keep showing up - for your kids, your pets, your garden. If acetaminophen helps you walk to the mailbox, that’s a win. If topical NSAIDs help you play piano again? Even better. No shame in stacking tools. We’re not failing if we need help - we’re being smart.
And hey - if you’re reading this and feeling overwhelmed? Start with one thing. One walk. One label read. One conversation with your doctor. You don’t need to fix everything today.
Jens Petersen
November 6, 2025 AT 22:32Acetaminophen is the pharmaceutical equivalent of a Band-Aid on a severed artery - it looks neat, it’s cheap, and it makes the doctor feel like they did something. Meanwhile, the real pathology - the chronic inflammation, the synovial degeneration, the metabolic dysfunction - is left to fester like a neglected garden. We’ve turned medicine into a customer service department: "Here’s your pain reliever, ma’am. Would you like fries with that?" Meanwhile, the patient is quietly dying inside their own joints. This isn’t treatment. It’s triage with a smile.
And don’t get me started on glucosamine. That’s not medicine - it’s a placebo with a fancy label and a $25 price tag. If you’re taking it hoping for structural repair, you’re not just wasting money - you’re delaying real intervention.
Keerthi Kumar
November 8, 2025 AT 08:07Let us pause, just for a moment, to honor the quiet dignity of those who rise each morning with pain - not because they want to, but because they must. In my culture, we say: "The body remembers what the mind tries to forget." Acetaminophen? It is not a cure. It is not even a solution. It is a bridge - a fragile, temporary bridge - over the chasm of suffering. And if it allows someone to hold their grandchild’s hand, to feel the sun on their face, to take one more step without screaming - then who are we to call it useless? We must not mistake the tool for the purpose. The purpose is presence. The tool is merely a whisper of relief in a storm that never stops.
John Concepcion
November 9, 2025 AT 21:57Oh wow, a whole article about acetaminophen and not one mention of Big Pharma? Shocking. Next you’ll tell me the sun rises in the east and water is wet. Of course the guidelines say it’s safe - they’re written by doctors who get free trips to Hawaii from the drug reps. Wake up, sheeple. Nobody gets rich selling exercise programs.
Caitlin Stewart
November 10, 2025 AT 21:19My mom’s rheumatologist told her the same thing: "Try it for three weeks. If you’re not moving better, we’re changing gears." She did. Didn’t work. We switched to diclofenac gel - and now she’s gardening again. No miracle. Just the right tool for the job. Thanks for the nudge to ask the right questions.