Introduction to Amebiasis
Amebiasis is a parasitic infection caused by the single-celled protozoan, Entamoeba histolytica. This infection primarily affects the intestines, but it can also spread to other organs like the liver, lungs, and brain. In this article, we will delve into the causes, symptoms, and treatment options for amebiasis. By understanding the condition, you can take steps to protect yourself and your loved ones from infection and seek appropriate medical care if needed.
Causes and Transmission of Amebiasis
The primary cause of amebiasis is the ingestion of the Entamoeba histolytica parasite. This can happen when a person consumes food or water contaminated with the parasite. The contamination often occurs due to poor sanitation practices and inadequate hygiene. In developing countries, amebiasis is more prevalent due to limited access to clean water and proper waste disposal systems.
Amebiasis can also be transmitted through direct contact with an infected person, for example, through oral-anal sexual contact. It's important to practice good hygiene and take precautions to avoid contracting or spreading the infection.
Common Symptoms of Amebiasis
Many people infected with the Entamoeba histolytica parasite may not experience any symptoms. However, for those who do, the symptoms can range from mild to severe. Some common symptoms of amebiasis include:
- Abdominal pain and cramping
- Diarrhea, which may be bloody or contain mucus
- Fatigue and weakness
- Nausea and vomiting
- Weight loss and loss of appetite
- Flatulence and bloating
- Fever
If the infection spreads to other organs, additional symptoms may arise, such as chest pain, breathing difficulties, and jaundice. If you suspect that you or a loved one may have amebiasis, it's important to seek medical attention promptly.
Diagnosing Amebiasis
Diagnosing amebiasis can be challenging, as the symptoms are similar to those of other gastrointestinal disorders. A healthcare provider will typically take a detailed history of your symptoms, travel history, and potential risk factors. They may also perform a physical examination to check for any signs of infection.
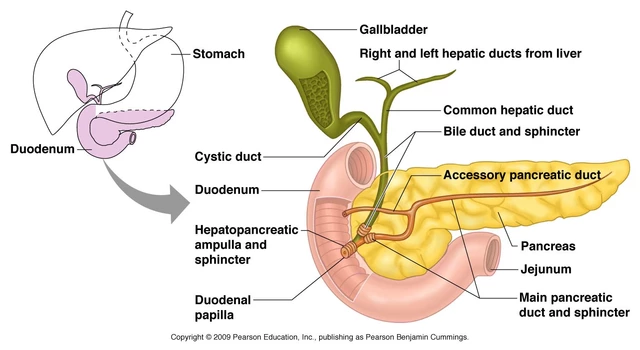
To confirm the diagnosis, your doctor may order laboratory tests, such as a stool sample analysis or blood tests. In some cases, imaging studies like ultrasound or CT scans may be necessary to assess the extent of the infection and any complications, such as liver abscesses.
Treatment Options for Amebiasis
Treating amebiasis typically involves the use of medications called antiprotozoal agents. These drugs work by targeting and killing the Entamoeba histolytica parasite. Some commonly prescribed medications for amebiasis include metronidazole, tinidazole, and paromomycin. Your healthcare provider will determine the most appropriate medication and dosage for your specific condition.
In addition to medication, it's crucial to maintain proper hydration, as diarrhea can lead to dehydration. Your doctor may recommend oral rehydration solutions or, in severe cases, intravenous fluids. If complications such as liver abscesses arise, additional treatments like drainage or surgery may be necessary.
Preventing Amebiasis
Prevention is key when it comes to amebiasis, especially in areas with a high risk of infection. Here are some steps you can take to protect yourself and your loved ones from contracting amebiasis:
- Practice good hand hygiene by washing your hands thoroughly with soap and water, especially after using the restroom and before preparing or eating food
- Drink only bottled or purified water, and avoid consuming tap water or ice made from tap water
- Peel or cook fruits and vegetables before consuming, as they may be contaminated with the parasite
- Avoid eating food from street vendors, as their hygiene practices may be questionable
- Use condoms during sexual encounters, particularly oral-anal contact
By following these precautions, you can greatly reduce your risk of contracting amebiasis.
Long-term Effects and Complications of Amebiasis
If left untreated, amebiasis can lead to several complications, including:
- Liver abscesses, which can cause severe pain, fever, and jaundice
- Perforation of the intestine, leading to peritonitis (a life-threatening infection of the abdominal cavity)
- Spread of the infection to other organs, such as the lungs, brain, or skin
- Malnutrition and weight loss due to poor absorption of nutrients
Early detection and treatment of amebiasis can help prevent these complications and ensure a smoother recovery.
Conclusion
Amebiasis is a potentially serious parasitic infection caused by the Entamoeba histolytica parasite. Understanding the causes, symptoms, and treatment options for this condition is crucial in order to protect yourself and your loved ones from infection. By practicing good hygiene, seeking prompt medical attention if you suspect infection, and following your healthcare provider's recommendations for treatment, you can effectively manage and prevent amebiasis.


Ellen Laird
May 13, 2023 AT 19:46One must simply eschew unpurifiedd water lest one succumb to such a paltry parasite.
rafaat pronoy
May 14, 2023 AT 09:40Staying hydrated while dealing with a nasty gut bug is key – keep a bottle handy and sip water or an ORS mix, it'll help you feel less crappy 😊.
sachin shinde
May 14, 2023 AT 23:33Observe the proper lexical constructions when referencing medical protocols; the phrase "use antiprotozoal agents" ought to be capitalized correctly in formal contexts. Moreover, the article’s occasional slip into colloquialism undermines its scientific gravitas. One must wield precision not only in treatment dosage but also in syntactic articulation. The misuse of "its" versus "it's" is a blatant transgression that cannot be ignored. While the content is valuable, the erratic punctuation-especially the errant semi‑colon-disrupts the reader's cognitive flow. Correcting these errors will elevate the discourse from pedestrian to scholarly. Emotional resonance, however, is achieved when the narrative conveys the urgency of early diagnosis, which the writer captures deftly. Yet the emotional undertone feels contrived, as if the writer feeds off others' anxieties. Such affective vampirism detracts from the objective analysis required in medical literature.
Leon Wood
May 15, 2023 AT 13:26Hey folks, remember you’ve got the power to beat this infection – follow the docs, eat right, and stay positive!
George Embaid
May 16, 2023 AT 03:20Friends from all backgrounds, let’s share safe water tips and support each other in navigating treatment options.
Meg Mackenzie
May 16, 2023 AT 17:13They don’t want you to know that the water‑filter industry is colluding with pharma to keep us dependent on pricey meds.
Shivaraj Karigoudar
May 17, 2023 AT 07:06From a holistic epidemiological standpoint, the multifactorial pathogenesis of amebiasis necessitates an integrative intervention framework that synthesizes both prophylactic sanitation measures and targeted pharmacotherapeutics. Firstly, the deployment of point‑of‑use chlorination devices, albeit seemingly rudimentary, has demonstrably reduced trophozoite viability in community water supplies; however, implementation fidelity remains heterogeneous across socio‑economic strata. Secondly, the pharmacokinetic profile of metronidazole, while extensively documented, invites scrutiny regarding its hepatic metabolism via the cytochrome P450 cascade, particularly in polymorphic populations where allele variance may precipitate subtherapeutic plasma concentrations. Thirdly, adjunctive therapy with paromomycin serves as a luminal agent, yet its poor systemic absorption mandates vigilant monitoring for nephrotoxic sequelae in renally compromised patients. Fourth, the sociocultural dimensions of oral‑anal sexual practices underscore the imperative for culturally competent educational modules that eschew stigmatization while promulgating barrier methods. Fifth, the emergence of resistance patterns, albeit sporadic, compels the scientific community to invest in novel anti‑amoebic scaffolds, leveraging high‑throughput screening of natural product libraries. Sixth, the role of host microbiome dysbiosis in modulating disease severity is an evolving frontier, suggesting probiotic supplementation as a potential adjunct. Seventh, in resource‑limited settings, the cost‑effectiveness of oral rehydration solutions versus intravenous fluid resuscitation must be calibrated against patient acuity scores. Eighth, the diagnostic algorithm-encompassing stool antigen detection, PCR assays, and imaging modalities-should be tiered to maximize sensitivity while minimizing invasive procedures. Ninth, community health worker training programs have shown efficacy in early case identification, reducing the incidence of hepatic abscesses. Tenth, policy‑level interventions, such as mandating water quality standards and subsidizing filtration technology, are essential to sustain long‑term disease control. Eleventh, ongoing surveillance data integration into geographic information systems (GIS) facilitates real‑time outbreak mapping, enabling rapid public health responses. Twelfth, interdisciplinary collaboration between gastroenterologists, infectious disease specialists, and public health officials is paramount to holistically address the disease burden. Thirteenth, patient adherence counseling, employing motivational interviewing techniques, bolsters therapeutic outcomes. Fourteenth, the psychosocial impact of chronic intestinal infections warrants mental health support services to mitigate stigma‑related distress. Finally, continuous research funding is critical to advance our collective understanding and ultimately eradicate amebiasis as a public health threat.