When you're on warfarin, even a simple antibiotic can throw your blood clotting off balance-sometimes with life-threatening results. It’s not just a theoretical risk. In real-world practice, antibiotics are responsible for 15-30% of all warfarin-related hospitalizations. That’s not rare. That’s common enough that every doctor, pharmacist, and patient on warfarin needs to know exactly how to handle it.
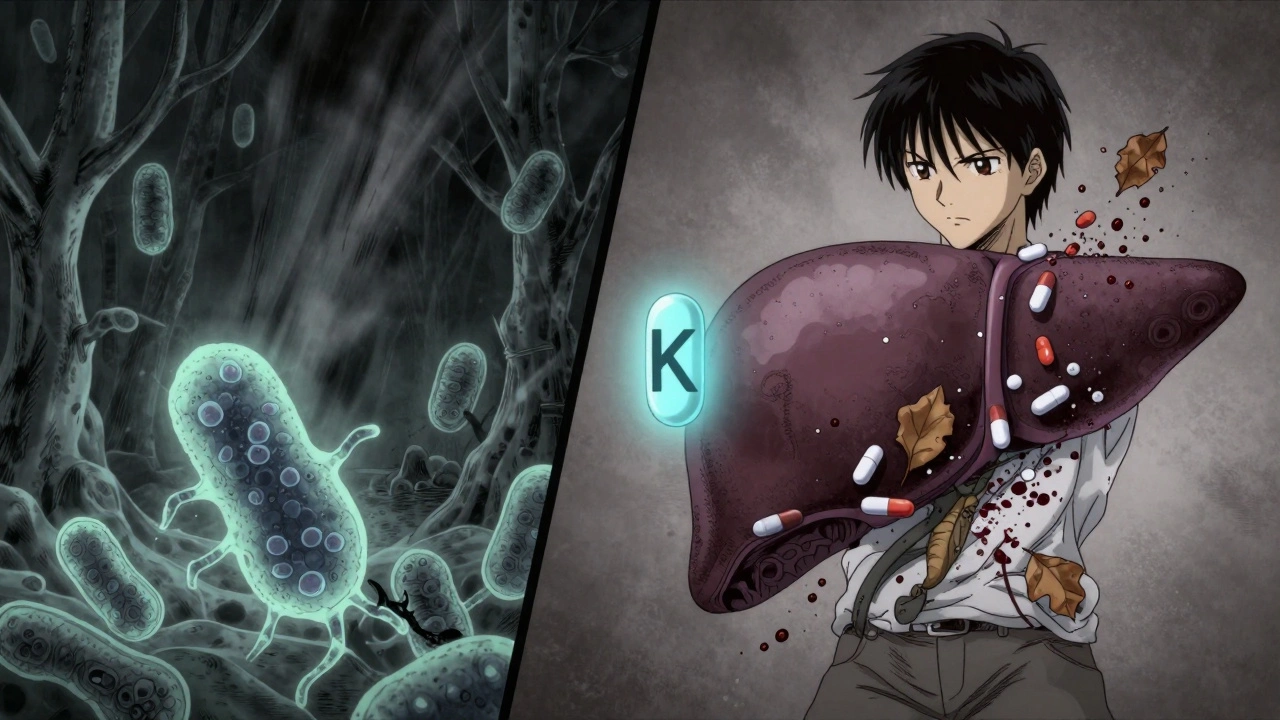
Warfarin works by blocking vitamin K, which your body needs to make clotting factors. But your gut bacteria also produce about 10-15% of your vitamin K. When you take certain antibiotics, you kill off those bacteria. That means less vitamin K, more warfarin effect, and a dangerous rise in INR. At the same time, some antibiotics slow down how your liver breaks down warfarin, causing levels to build up. Either way, your INR can spike into the danger zone-above 4.0-where major bleeding risk jumps 4 to 8 times.
Which Antibiotics Are the Biggest Risks?
Not all antibiotics are created equal when it comes to warfarin. Some barely touch your INR. Others? They’re ticking time bombs.
High-risk antibiotics include:
- Ciprofloxacin and levofloxacin (fluoroquinolones): These are the worst offenders. Ciprofloxacin can push INR from 2.5 to 4.1 in under a week. Bleeding risk increases by more than double.
- Bactrim (sulfamethoxazole/trimethoprim): Causes INR to rise by an average of 1.8 units within five days. Commonly prescribed for UTIs, it’s one of the top three antibiotics linked to warfarin emergencies.
- Erythromycin (macrolide): Strongly inhibits liver enzymes. Increases bleeding risk by 2.3 times.
- Amoxicillin/clavulanate (Augmentin): Doesn’t affect liver enzymes much-but wipes out gut bacteria. INR rises by about 1.2 units on average.
- Cefotetan and cefoperazone (cephalosporins): These have a special chemical group (N-methylthiotetrazole) that blocks vitamin K activity directly. INR can jump 1.5 to 2.2 units.
On the flip side, some antibiotics are mostly safe:
- Azithromycin (Zithromax): Minimal enzyme interaction. Bleeding risk barely moves.
- Ceftriaxone: Very low interaction risk. INR change is usually less than 0.3 units.
- Nitrofurantoin and fosfomycin: No significant effect on INR. Often the go-to choices for UTIs in patients on warfarin.
And then there’s rifampin-the opposite problem. It speeds up warfarin breakdown. INR can crash below 1.5. That means clots. Strokes. Pulmonary embolisms. You have to increase your warfarin dose by 50-100% when starting rifampin.
When Do INR Spikes Happen-and How Long Do They Last?
Timing matters. If you think an INR spike happens right away, you’re wrong. The body doesn’t react that fast.
CYP enzyme interactions (like with ciprofloxacin or erythromycin) show up in 48 to 72 hours. That’s why the first INR check after starting antibiotics should be within 72 hours.
Gut flora disruption (from amoxicillin, Bactrim, or cephalosporins) takes longer. It hits around day 5 to 7. And here’s the kicker-it doesn’t disappear when you stop the antibiotic. Your gut bacteria need 7 to 10 days to recover. That means your INR can stay high for a full week after the last pill.
That’s why guidelines say: check INR after you finish the antibiotic too. Not just when you start it. Bleeding risk peaks between days 8 and 14 of antibiotic use. That’s when most hospitalizations happen.
What Should You Do? A Clear Action Plan
If you’re on warfarin and your doctor prescribes an antibiotic, don’t just take it. Do this:
- Ask which antibiotic they’re prescribing. If it’s ciprofloxacin, Bactrim, or amoxicillin/clavulanate, push back. Ask if there’s a safer alternative-like azithromycin or nitrofurantoin.
- Get an INR test within 72 hours of starting the antibiotic. Don’t wait for your next scheduled check.
- Test again 3 to 5 days after starting and then weekly until the antibiotic ends.
- Test again 3 to 5 days after finishing. The danger doesn’t end when the pills do.
- Know the bleeding signs: Unexplained bruising, nosebleeds that won’t stop, red or black stools, pink or brown urine, severe headaches, dizziness, or swelling under the skin. Call your anticoagulation clinic immediately if you see any of these.
- Don’t adjust your dose yourself. Only your provider should change your warfarin. But if your INR is over 4.0, they may reduce your dose by 20-30%-especially with high-risk antibiotics.
For high-risk antibiotics like ciprofloxacin or Bactrim, many clinics start by reducing the warfarin dose by 20-30% right away. For gut-flora disruptors like amoxicillin/clavulanate, they wait and watch-only adjusting if INR climbs too high. For rifampin, they increase the dose upfront.
Why Pharmacist-Led Care Works Better
Studies show that when pharmacists manage warfarin therapy during antibiotic use, bleeding complications drop by 37%. Why? Because pharmacists are trained to spot these interactions. They track INR trends. They know which antibiotics are dangerous. They call patients when results come back abnormal.
Most doctors are busy. They might not remember that your warfarin dose needs a reset after a course of antibiotics. But a pharmacist? They’ll flag it. They’ll call you. They’ll adjust your dose based on real data-not guesswork.
If your clinic doesn’t have a pharmacist on staff, ask if you can schedule a medication review. It’s free in many places. And it could save your life.
What About Genetic Testing?
Some people have a genetic variant in the CYP2C9 gene-called *2 or *3-that makes them extra sensitive to warfarin. If you have one of these, your INR can spike 2.4 times higher than normal when you take an interacting antibiotic.
There’s a new approach: genotype-guided dosing. In the 2023 WARF-GEN trial, patients who had their CYP2C9 and VKORC1 genes tested before starting antibiotics had 41% fewer INR spikes than those who didn’t. It’s not routine yet-but it’s coming fast.
If you’ve been on warfarin for years and keep having unstable INRs, ask your doctor about genetic testing. It might explain why you’ve had problems before-and help prevent them in the future.

The Bottom Line: Don’t Assume It’s Safe
There’s no such thing as a "safe" antibiotic for warfarin users without checking. Even antibiotics that seem mild-like amoxicillin-can cause big INR swings. And the risk doesn’t go away when the antibiotic ends.
The key is vigilance. Not fear. You don’t have to avoid antibiotics. You just have to manage them smartly. Test early. Test often. Know the signs. Talk to your pharmacist. Don’t let a simple infection turn into a bleeding emergency.
Warfarin isn’t a drug you can take on autopilot. Not anymore. Not with antibiotics involved. The data is clear. The guidelines are solid. What’s missing? Action.
Can I take ibuprofen or aspirin while on warfarin and antibiotics?
No. Both ibuprofen and aspirin increase bleeding risk on their own-and when combined with warfarin and an antibiotic, the danger multiplies. Even low-dose aspirin can raise your risk of stomach bleeding. Use acetaminophen (Tylenol) for pain instead. Always check with your provider before taking any new medication, even over-the-counter ones.
How often should I check my INR if I’m on antibiotics?
Check within 72 hours of starting the antibiotic, then every 2-3 days for high-risk drugs like ciprofloxacin or Bactrim. For moderate-risk antibiotics like amoxicillin, check every 5-7 days. After finishing the antibiotic, check again 3-5 days later. Some patients need weekly checks for up to two weeks after stopping. Your provider will tailor this based on your history and the antibiotic used.
What if my INR is over 5.0?
An INR over 5.0 is dangerous. You’re at high risk of spontaneous bleeding. Do not take your next warfarin dose. Call your anticoagulation clinic immediately. They may give you vitamin K (orally or intravenously) to reverse the effect. In severe cases, you may need fresh frozen plasma. Never wait to see if it "goes down on its own."
Can I eat more vitamin K to fix a high INR?
Eating more vitamin K (like leafy greens) can help stabilize your INR over time-but it won’t fix a sudden spike caused by antibiotics. The problem isn’t dietary vitamin K-it’s your gut bacteria being wiped out and your liver slowing down warfarin metabolism. Vitamin K supplements should only be used under medical supervision. Too much can make your INR too low and increase clot risk.
Are new antibiotics like tedizolid safe with warfarin?
Yes. Tedizolid, a newer antibiotic for skin infections, has been shown in studies to cause almost no change in INR-only a +0.2 unit average increase. It’s considered low-risk. But even low-risk drugs need monitoring. Don’t assume safety without checking your INR.
What If I’m Still Confused?
Take this simple rule: if you’re on warfarin and your doctor says you need an antibiotic, say: "Which one are you prescribing? Is it safe with warfarin? Can we check my INR before and after?" If they hesitate or don’t know, ask for a pharmacist consult. It’s your life. You have the right to ask.
Antibiotics save lives. Warfarin saves lives. But together? Without careful management, they can kill. The science is clear. The protocols exist. What you do next matters more than anything else.



Harriet Wollaston
December 13, 2025 AT 12:39I was on warfarin for AFib and got prescribed cipro for a UTI last year-didn’t know any of this. My INR jumped to 5.8 and I ended up in the ER with a nosebleed that wouldn’t stop. I still get nervous every time I get sick now. But honestly? This post saved my life. I’m telling everyone I know who’s on blood thinners to read this.
Hamza Laassili
December 15, 2025 AT 02:29OMG!!! I JUST TOOK BACTRIM FOR MY BLADDER INFECTION AND I’M ON WARFARIN!!! I’M GONNA DIE!!! I’M CALLING MY DOCTOR RIGHT NOW!!!
Constantine Vigderman
December 16, 2025 AT 20:12Bro this is wild 😱 I just found out my grandma’s on warfarin and her doc gave her amoxicillin last week-no INR check, nada. I’m gonna print this out and tape it to her fridge. Seriously, if you’re on blood thinners, you gotta be your own advocate. My uncle had a stroke because they didn’t adjust his dose after antibiotics. Don’t be him. Check your INR. Talk to the pharmacist. Don’t just trust the script.
Cole Newman
December 17, 2025 AT 01:39You guys are overreacting. I’ve been on warfarin for 12 years and I’ve taken cipro like 5 times. Never had a problem. Your INR’s probably just off because you’re eating kale or drinking grapefruit juice. Stop being paranoid. If your doctor says it’s fine, it’s fine. Stop reading Reddit like it’s medical school.
Casey Mellish
December 17, 2025 AT 08:25As an Aussie who’s seen the anticoagulation clinics here, I can confirm-pharmacist-led management cuts bleeding events by nearly half. We have dedicated anticoagulation pharmacists who call patients after every INR test, especially when antibiotics are involved. It’s standard. Here in the US, why are we still leaving this to overworked GPs? We need this model nationwide. It’s not just good practice-it’s cost-effective and life-saving.
kevin moranga
December 19, 2025 AT 08:21Let me tell you something-this isn’t just about antibiotics. It’s about how we treat people on warfarin like they’re ticking time bombs instead of human beings who deserve clear, consistent care. I’ve had patients cry because their doctor didn’t warn them about Bactrim. I’ve had people skip their INR checks because they were too scared to call. This post? It’s not just info-it’s a lifeline. If you’re on warfarin, you’re not broken. You’re just playing a game with higher stakes. And now you’ve got the playbook. Keep checking. Keep asking. Keep living. You’ve got this.
Alvin Montanez
December 20, 2025 AT 01:42People need to stop being lazy. This isn’t rocket science. If you’re on warfarin, you should already know the risks. You should already be tracking your INR. You should already be asking about drug interactions. You don’t need a Reddit post to tell you that antibiotics can kill you. You need to take responsibility for your own health. Stop waiting for someone else to protect you. You’re an adult. Act like it. And if you’re still on warfarin after all this? Good. But don’t blame the system-blame yourself for not being informed.
Jamie Clark
December 21, 2025 AT 12:38Here’s the uncomfortable truth: medicine isn’t about safety. It’s about profit. Antibiotics are cheap. INR tests are expensive. Pharmacists are underpaid. Patients are ignored. This post exposes a system that treats warfarin patients like collateral damage. We’re not talking about rare side effects-we’re talking about predictable, preventable deaths. And the system lets them happen because it’s easier than changing. So yes, check your INR. But also ask: why does this even need to be a warning? Why isn’t this protocol built into every EHR? Why aren’t we forcing pharmacies to flag these interactions? The answer isn’t education. It’s accountability.
Keasha Trawick
December 23, 2025 AT 03:33Okay, so picture this: your gut bacteria are these tiny, sweaty little ninjas, minding their own business, churning out vitamin K like it’s a 24/7 smoothie bar. Then-BAM-ciprofloxacin walks in like a neon-lit demolition crew, screaming "EVERYBODY OUT!" and wiping out your entire microbial workforce. Suddenly, your liver’s like, "Wait, why is warfarin still here?!" and it just… accumulates. Like a toxic hoarder. And now your INR’s soaring, your blood’s basically tap water, and you’re wondering why your gums are bleeding during a sneeze. This isn’t science-it’s a horror movie written by a pissed-off biochemist. And the villain? A $12 antibiotic prescription. 🤯
Bruno Janssen
December 24, 2025 AT 12:46I’ve been on warfarin for 8 years. I never told anyone how scared I am. Every time I get sick, I panic. I don’t know which antibiotics are safe. I don’t know if I should call my doctor or just wait. I just… sit there. And read. And hope. I didn’t know about the 7-10 day lag after antibiotics. I thought once the pills were done, I was safe. I wasn’t. I just… thank you. For writing this. I’m printing it.