Beta-Blocker Comparison Tool
Compare beta-blockers based on receptor targeting, clinical uses, side effects, and patient feedback to understand why your doctor might choose one over another.
Select two beta-blockers to compare
Not all beta-blockers are the same. Even though they all block adrenaline, the differences between them can mean the difference between relief and side effects, between better heart function and no change at all. If you’ve been prescribed a beta-blocker and wonder why your doctor chose one over another, it’s not random. It’s based on how each drug behaves in your body - and what your body needs.
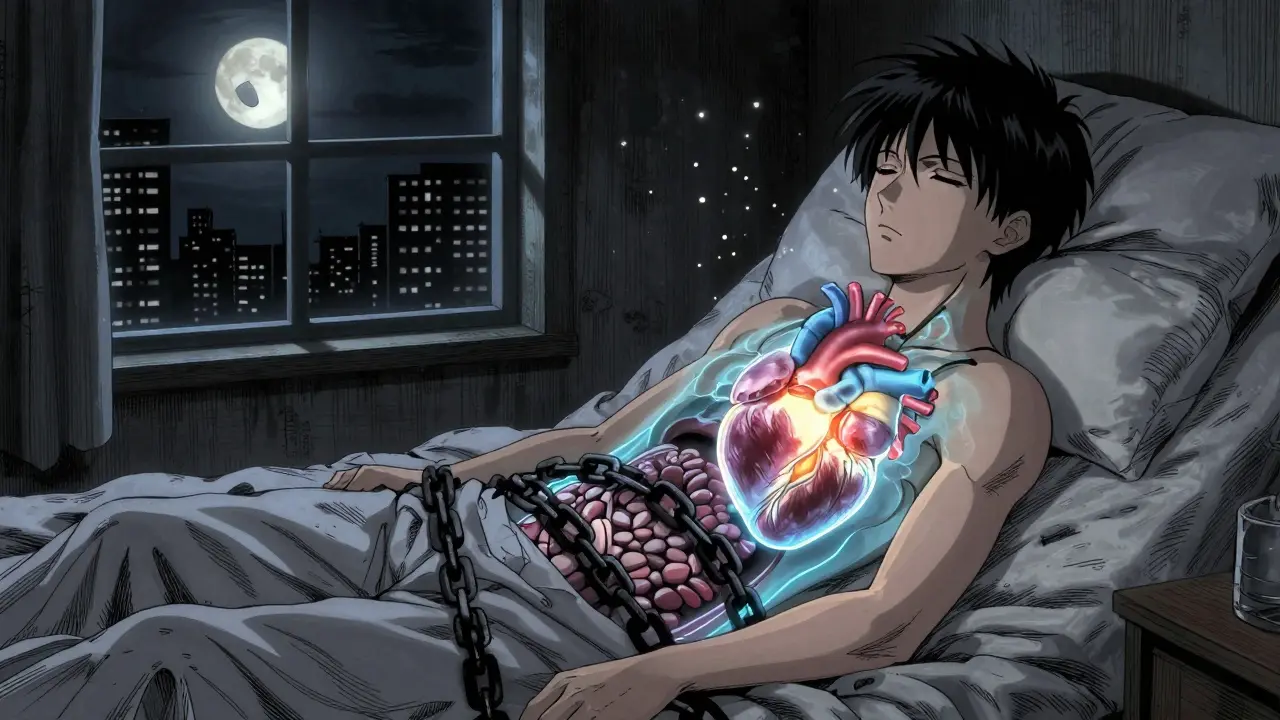
What Beta-Blockers Actually Do
Beta-blockers stop adrenaline from overworking your heart. Adrenaline - also called epinephrine - is your body’s natural stress signal. When you’re scared, stressed, or exercising, it tells your heart to beat faster and harder. That’s fine in emergencies. But if your heart is already damaged, or if you have high blood pressure, that constant push can make things worse.
Beta-blockers act like a mute button on that signal. They bind to beta receptors in your heart and blood vessels, blocking adrenaline from turning up the volume. The result? Slower heart rate, lower blood pressure, less forceful contractions. That’s why they’re used after heart attacks, in heart failure, for irregular heartbeats, and sometimes for migraines or tremors.
But here’s the catch: beta receptors aren’t all the same. There are three types - beta-1, beta-2, and beta-3 - and different drugs hit them in different ways. That’s where the real differences begin.
First-Generation: The Broad Sweep
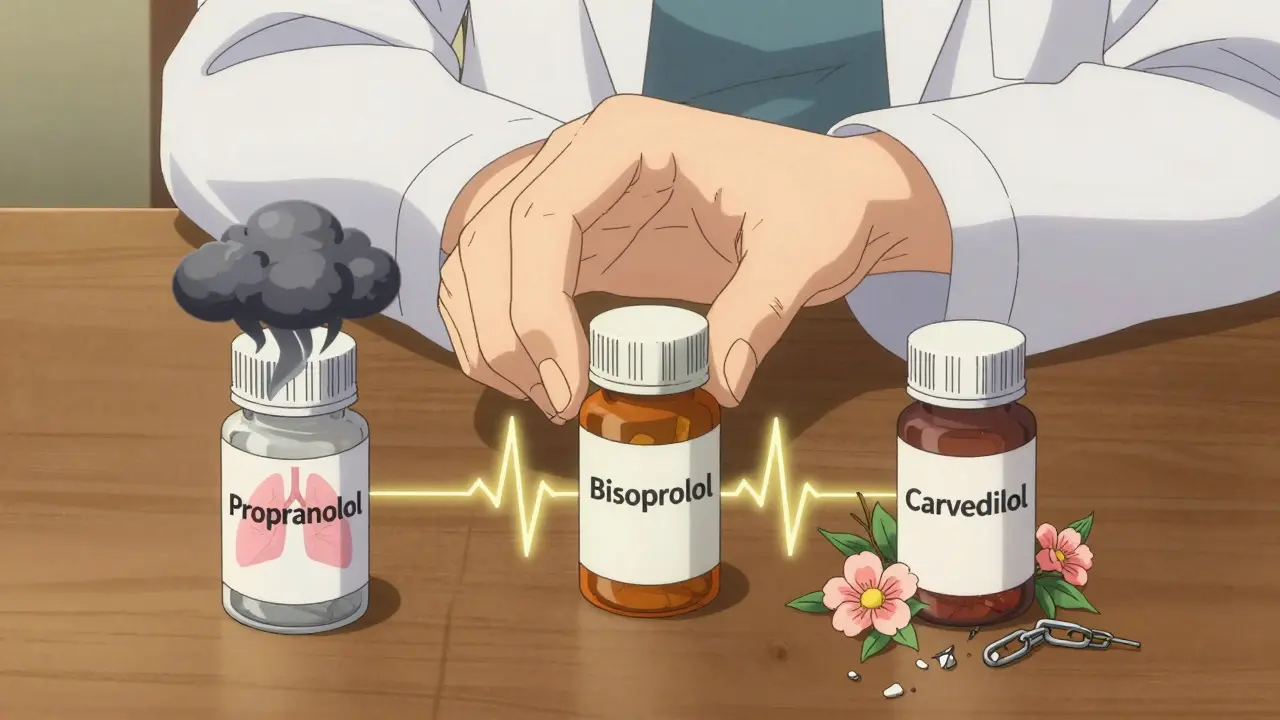
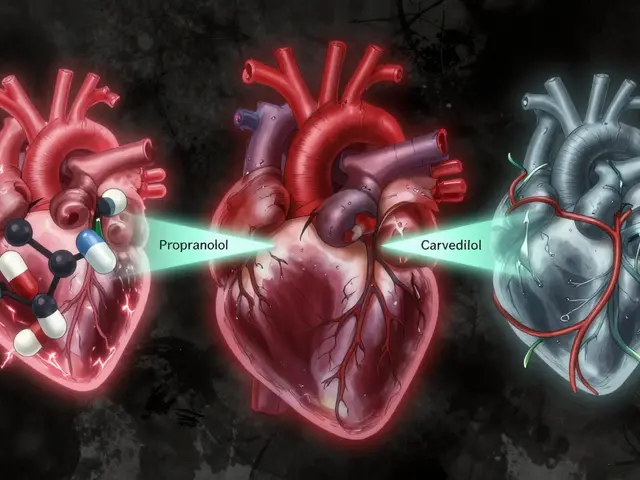
Propranolol was the first beta-blocker, introduced in the 1960s. It blocks both beta-1 and beta-2 receptors - everywhere. That’s why it works for heart conditions, but also why it can cause trouble.
Beta-2 receptors are in your lungs, blood vessels, and muscles. Block them, and you risk tightening airways. That’s why people with asthma or COPD are usually told to avoid propranolol. It can trigger wheezing or even an attack. It also reduces blood flow to your hands and feet, making them feel cold. Some users report fatigue, sleep problems, or even low mood.
Propranolol is still used - especially for tremors, anxiety-related palpitations, and certain arrhythmias. But because it’s nonselective and has a short half-life (meaning it wears off quickly), it often needs to be taken two or three times a day. That makes adherence harder. Its average rating on patient sites is 6.2 out of 10, with nearly 4 in 10 reporting moderate to severe side effects.
Second-Generation: Targeted for the Heart
Doctors wanted the heart benefits without the lung side effects. That led to beta-1 selective blockers - drugs like metoprolol, atenolol, bisoprolol, and esmolol. These mainly stick to beta-1 receptors, which are mostly in the heart. That makes them safer for people with mild asthma or COPD - though caution is still needed.
Metoprolol comes in two forms: tartrate (Lopressor) and succinate (Toprol XL). Tartrate is short-acting and needs twice-daily dosing. Succinate is extended-release, taken once a day. Many patients prefer the once-daily version. A 2022 Cleveland Clinic survey found 85% of heart failure patients stuck with carvedilol or metoprolol succinate because they were easier to manage.
Bisoprolol is another popular choice. It’s highly selective, long-lasting, and has fewer reports of fatigue or depression than propranolol. Its average rating is 7.1 out of 10. Atenolol, while cheap and widely used, doesn’t offer the same heart protection in heart failure as the newer agents. It’s mostly used for high blood pressure, but even there, it’s no longer first-line.
Third-Generation: More Than Just Blocking
Then came the game-changers: carvedilol and nebivolol. These aren’t just blockers - they’re multi-tools.
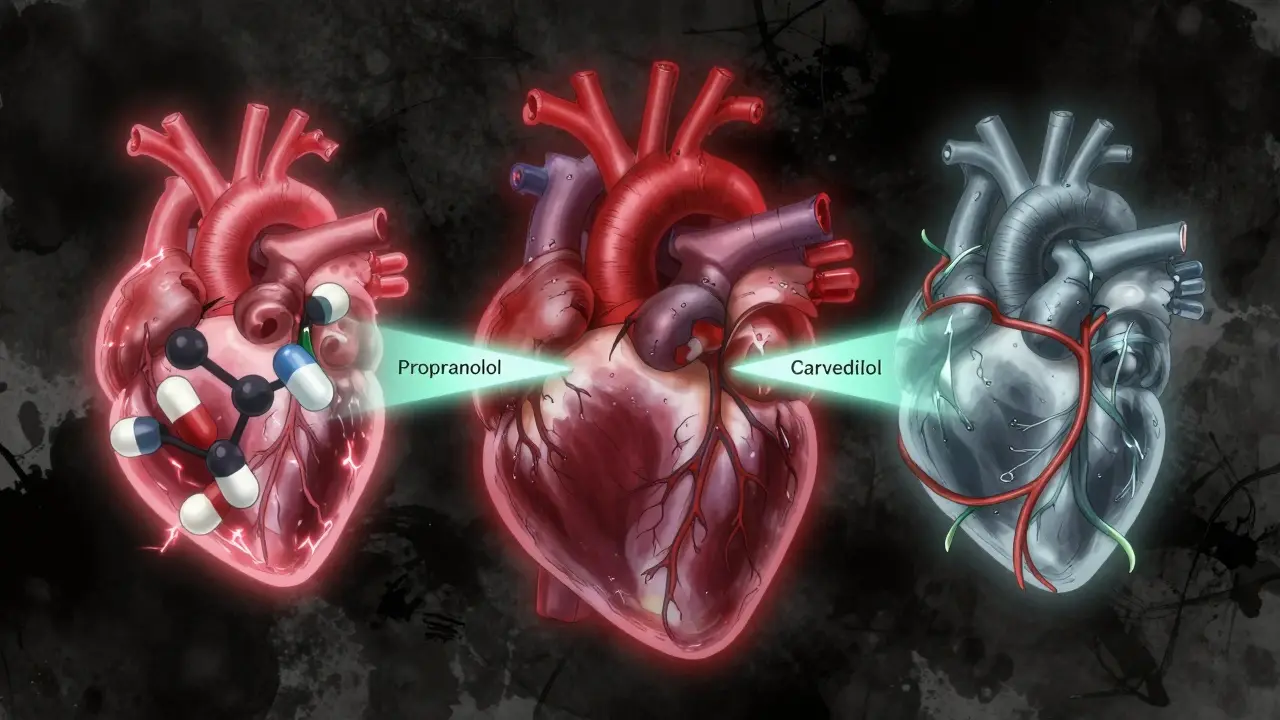
Carvedilol blocks beta-1 receptors, but also alpha-1 receptors. That means it doesn’t just slow the heart - it relaxes blood vessels. This reduces resistance in your arteries, lowering blood pressure even more. In the landmark US Carvedilol Heart Failure Study (1996), it cut death risk by 35% compared to placebo. That’s why it’s a cornerstone in heart failure treatment today. It also has strong antioxidant effects, reducing oxidative stress in heart tissue by 30-40% in lab studies. That helps prevent further damage.
Nebivolol is even more unique. It blocks beta-1 receptors and activates beta-3 receptors, which trigger nitric oxide production. Nitric oxide is a natural vasodilator - it opens up your blood vessels. This gives it an extra edge: it lowers blood pressure without making you feel tired or cold. In fact, some men report improved sexual function on nebivolol compared to older beta-blockers. A Reddit thread from a cardiac nurse in 2023 noted 65% of male patients over 50 saw better erectile function on nebivolol than on metoprolol or atenolol.
Both carvedilol and nebivolol are now recommended by the European Society of Cardiology for heart failure with reduced ejection fraction. They’re not just alternatives - they’re preferred.
Why One Size Doesn’t Fit All
Choosing the right beta-blocker isn’t about what’s newest or most expensive. It’s about matching the drug to the person.
If you have asthma or COPD, avoid nonselective blockers like propranolol. Stick to bisoprolol or metoprolol succinate - but even then, start low and go slow.
If you have heart failure, carvedilol or nebivolol are the top choices. They don’t just manage symptoms - they extend life. Studies show carvedilol reduces hospital stays and death risk more than older drugs.
If you’re older and have high blood pressure alone, beta-blockers aren’t the first move anymore. ACE inhibitors, ARBs, or calcium channel blockers work better at protecting your arteries. Beta-blockers are now reserved for when you have another condition - like a prior heart attack, arrhythmia, or heart failure.
And if you’re struggling with fatigue, cold hands, or low mood on a beta-blocker, don’t just accept it. Talk to your doctor. Switching from propranolol to bisoprolol or nebivolol often improves quality of life without losing effectiveness.
What You Need to Watch For
Beta-blockers aren’t dangerous if used right. But there are key risks.
- Don’t stop suddenly. Abruptly quitting can spike your heart rate and blood pressure, raising your risk of heart attack by 300% in the first 48 hours. Always taper under medical supervision.
- Watch for low heart rate. If your pulse drops below 50 bpm and you feel dizzy or faint, call your doctor. You might need a dose adjustment.
- Watch for drug interactions. Beta-blockers can reduce the effect of asthma inhalers like albuterol. If you’re on a nonselective beta-blocker, your inhaler might not work as well.
- Check kidney and liver function. Some beta-blockers are cleared by the liver (like carvedilol), others by the kidneys (like atenolol). If you have kidney disease, your doctor may avoid atenolol.
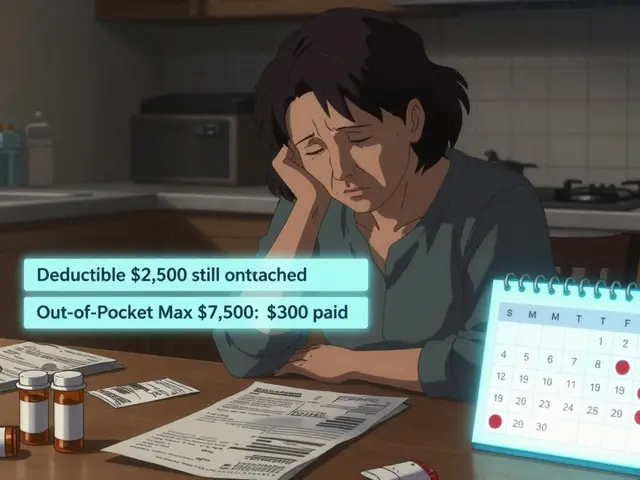
Also, dosing matters. Carvedilol must be titrated slowly - starting at 3.125 mg twice daily and increasing every 2 weeks. Rushing this can cause low blood pressure and dizziness. Bisoprolol can be increased faster. Nebivolol is usually started at 5 mg daily. Metoprolol succinate is taken once daily, while metoprolol tartrate needs twice-daily dosing. Confusing the two can lead to under- or overdosing.
What’s New and What’s Coming
The beta-blocker field isn’t standing still. In 2023, the FDA approved entricarone - a new drug that combines beta-3 activation with beta-1 blockade for heart failure with preserved ejection fraction. Early trials showed a 22% drop in hospitalizations.
By 2024, combination pills like nebivolol plus valsartan (an ARB) are expected to hit the market. These aim to simplify treatment for patients needing both blood pressure control and heart protection.
Even more exciting? Genetic testing. The GENETIC-BB trial is testing whether your DNA can predict which beta-blocker will work best for you. Some people metabolize drugs faster. Others are more sensitive. Tailoring based on genes could make beta-blocker therapy more precise than ever.
Bottom Line
Beta-blockers are not interchangeable. Propranolol isn’t the same as carvedilol. Metoprolol tartrate isn’t the same as nebivolol. The right choice depends on your condition, your other health issues, your age, and even your lifestyle.
If you’re on a beta-blocker and not feeling well - tired, cold, depressed, or short of breath - ask if there’s a better option. Many patients feel dramatically better after switching to a more targeted agent.
And if you’re newly prescribed one, ask your doctor: Why this one? What’s it doing that others don’t? Understanding the difference isn’t just helpful - it’s essential for getting the most benefit and avoiding harm.
Are beta-blockers still used for high blood pressure?
Yes, but not as a first choice for most people. Guidelines from the Mayo Clinic and ACC/AHA now recommend ACE inhibitors, ARBs, or calcium channel blockers as initial treatment for simple high blood pressure. Beta-blockers are reserved for patients who also have heart disease, a prior heart attack, arrhythmias, or heart failure. They’re less effective at lowering central aortic pressure - the kind that damages arteries over time - compared to other drugs.
Can I take a beta-blocker if I have asthma?
It depends. Nonselective beta-blockers like propranolol can trigger dangerous bronchospasm in people with asthma. But cardioselective beta-blockers like bisoprolol or metoprolol succinate are generally safer because they target the heart more than the lungs. Even then, they’re used cautiously, starting with low doses and monitoring closely. Never take a beta-blocker for asthma without your doctor’s approval.
Why is carvedilol better than metoprolol for heart failure?
Carvedilol blocks both beta and alpha receptors, which helps relax blood vessels and reduce strain on the heart. It also has antioxidant properties that protect heart cells from damage. In clinical trials, carvedilol reduced death risk by 35% compared to placebo, while metoprolol tartrate showed a smaller benefit. Metoprolol succinate (extended-release) is also effective, but carvedilol has more robust evidence for long-term survival in heart failure patients.
Do beta-blockers cause depression or fatigue?
Some people report fatigue, low energy, or low mood - especially with older drugs like propranolol. Studies show up to 33% of users experience exercise intolerance, and 19% report depression. Newer agents like nebivolol and bisoprolol have much lower rates of these side effects. If you’re feeling unusually tired or down, talk to your doctor. Switching drugs often helps without losing heart protection.
How long does it take for beta-blockers to work?
For heart rate and blood pressure, you might notice changes within hours to days. But for heart failure or after a heart attack, the real benefits - like reduced hospitalizations and longer life - take weeks to months. Dosing usually starts low and increases slowly over 4 to 12 weeks. Don’t expect instant results. The goal is long-term protection, not quick fixes.
Can beta-blockers affect sexual function?
Yes - but not all of them. Older beta-blockers like propranolol and atenolol are linked to erectile dysfunction in up to 30% of men. Newer agents like nebivolol, however, may actually improve sexual function. This is because nebivolol boosts nitric oxide, which helps with blood flow. If sexual side effects are a concern, ask your doctor about switching to nebivolol or carvedilol.

Rachel Kipps
February 3, 2026 AT 18:56I’ve been on metoprolol for 3 years now and honestly? I thought it was just a heart pill. Didn’t realize it was so specific. My hands used to be freezing all the time, and I felt like a zombie after lunch. Switched to bisoprolol last year and it’s like I got my life back. No more cold fingers, no more 3pm crashes. My doctor never explained why they picked it, though. Just said ‘this one’s better.’ Now I get why.
Wendy Lamb
February 4, 2026 AT 23:19My mom’s on carvedilol. She had a heart attack last year. The fatigue? Gone. The swelling? Reduced. The doctor said it’s not just slowing her heart-it’s healing it. I didn’t know beta-blockers could do that. Thanks for breaking this down. So many people just take pills without knowing why.
Justin Fauth
February 5, 2026 AT 08:08So now we’re giving fancy names to drugs that just slow your heart? What’s next, ‘anti-stress’ vitamins that come in gold-plated bottles? We got people in this country dying because they can’t afford insulin, and we’re spending millions on nebivolol because some guy in a lab said it ‘boosts nitric oxide.’ Get real.
Amit Jain
February 6, 2026 AT 12:42Simple truth: if you have high blood pressure only, don't start with beta-blocker. Use ACE or calcium blocker first. Beta-blockers are for heart damage, not just pressure. Many doctors still prescribe them wrong. I work in clinic. Saw this too many times. Patient comes, we switch to bisoprolol, they feel better. Easy fix.
rahulkumar maurya
February 7, 2026 AT 22:23How delightful that you’ve reduced a complex pharmacological landscape to a BuzzFeed-style bullet list. The fact that you mention the US Carvedilol Heart Failure Study without citing the NEJM paper suggests a superficial grasp of clinical evidence. Nebivolol’s beta-3 agonism? Fascinating, yes-but do you understand the downstream cGMP signaling cascade? Or are you just here to nod along while your doctor ups your dose? I’m not impressed.
Jamillah Rodriguez
February 9, 2026 AT 15:42Okay but why does everyone on here sound like a medical textbook? 😩 I just want to know if I can still drink coffee. Also, my ex says I’m ‘less fun’ since I started taking metoprolol. Is that a side effect or just him being dramatic? 🤷♀️
Susheel Sharma
February 11, 2026 AT 10:16Propranolol users are the reason medicine is broken. You think you’re ‘anxious’? Nah. You’re just weak. And now you want a ‘better’ beta-blocker? Grow up. Nebivolol for ED? LOL. Next you’ll be asking for a pill that makes your cat love you. Meanwhile, real patients in India are getting generic atenolol for $0.02/day. You people are spoiled.
Janice Williams
February 12, 2026 AT 12:35How dare you suggest that nebivolol improves sexual function? This is precisely the kind of pharmaceutical marketing masquerading as science that has led to the collapse of public trust in medicine. Nitric oxide? Please. It’s a vasodilator, not a love potion. And who approved this narrative? A drug rep? A TikTok influencer? This is dangerous misinformation.
Roshan Gudhe
February 13, 2026 AT 08:15It’s funny how we treat drugs like they’re magic wands. Beta-blockers don’t fix anything-they just quiet the noise. The heart still knows it’s broken. Maybe the real question isn’t which drug works best-but why we keep trying to silence symptoms instead of asking why the system is screaming in the first place. We treat the heart like a machine, not a living thing. And we wonder why people feel empty after taking pills for years.
Prajwal Manjunath Shanthappa
February 14, 2026 AT 07:35Let me be perfectly clear: if you’re taking metoprolol tartrate twice daily, you’re doing it wrong. You’re either being underdosed, misinformed, or both. And if you’re not on extended-release, you’re not getting the full benefit. And don’t even get me started on the fact that you’re probably not monitoring your HR daily. You’re not managing your condition-you’re just hoping it goes away. Pathetic.
Antwonette Robinson
February 16, 2026 AT 01:46Wow. So after all that, the takeaway is… don’t take propranolol if you have asthma? Groundbreaking. I’m sure your doctor didn’t already know that. Also, nebivolol helps with ED? So… what, I should ask for it like I’m ordering a latte? ‘Hi, can I get a 5mg nebivolol with extra nitric oxide, please?’