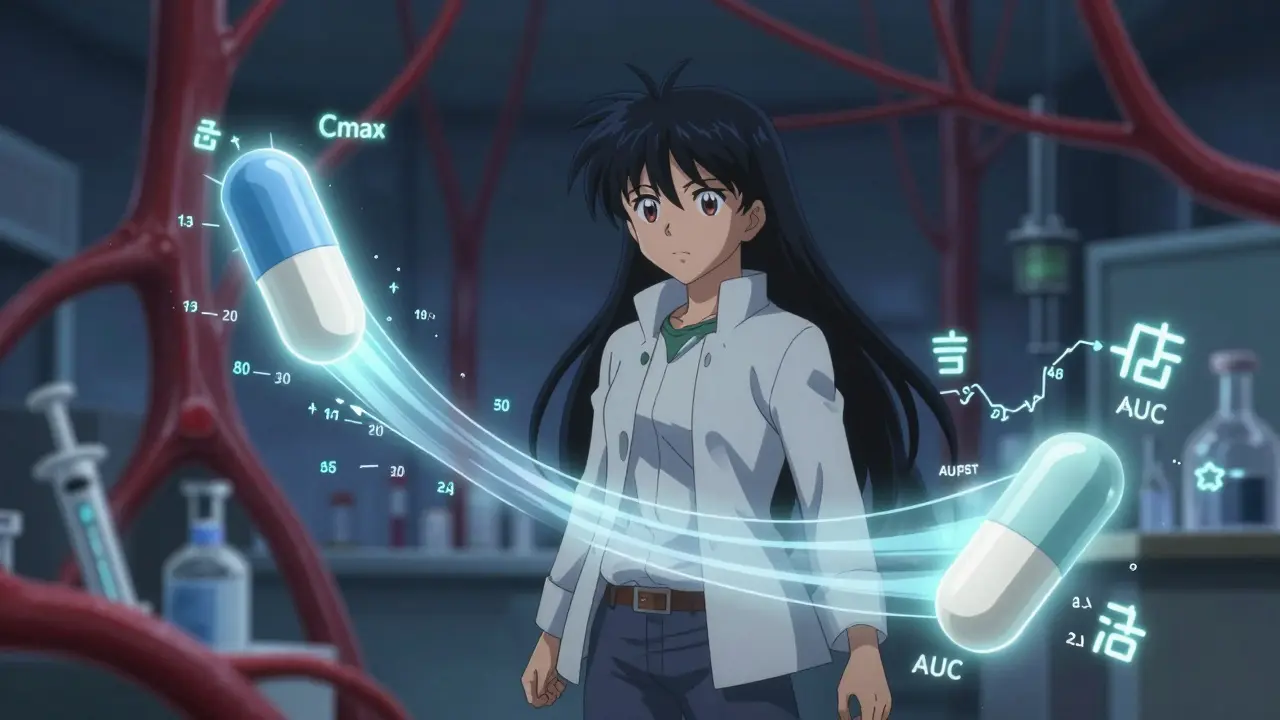
When you pick up a generic pill from the pharmacy, you expect it to work just like the brand-name version. But how do regulators know it’s truly the same? The answer lies in two numbers: Cmax and AUC. These aren’t just lab jargon-they’re the backbone of bioequivalence testing, the system that ensures generic drugs are safe and effective replacements.
What Cmax and AUC Actually Measure
Cmax stands for maximum concentration. It’s the highest level a drug reaches in your bloodstream after you take it. Think of it like the peak of a wave-how high does the drug surge when it hits its strongest point? This matters because some drugs only work if they hit a certain high enough concentration. For example, painkillers like ibuprofen need to reach a sharp peak to block pain signals quickly. If the generic version doesn’t hit the same peak, you might not feel relief fast enough-or worse, you might get side effects if it spikes too high.
AUC, or area under the curve, tells you the total amount of drug your body is exposed to over time. Imagine drawing a graph of drug levels in your blood from the moment you swallow the pill until it’s all cleared out. AUC is the area under that line. It’s not about the peak-it’s about the whole ride. For drugs that need to stay in your system for hours, like antibiotics or blood pressure meds, AUC is the key. If your AUC is too low, the drug won’t work long enough. Too high, and you risk toxicity.
Together, Cmax and AUC give regulators a full picture: how fast the drug gets into your blood (Cmax), and how much of it you get over time (AUC). If both match the original drug, the generic is considered bioequivalent.
Why Both Numbers Are Non-Negotiable
Some people think if AUC matches, Cmax doesn’t matter. That’s a dangerous assumption. The U.S. FDA and European Medicines Agency (EMA) both require both values to pass the same strict test. Why? Because they measure different things-and both affect how a drug behaves in your body.
Take warfarin, a blood thinner with a very narrow safety window. A tiny difference in Cmax could cause a dangerous spike in anticoagulation, leading to bleeding. But if AUC is too low, you’re not protected from clots. One study from the FDA showed that even when AUC was within range, a 15% drop in Cmax led to increased clotting events in patients switching generics.
Another example: levothyroxine, used for thyroid conditions. Small changes in absorption can throw off hormone levels, causing fatigue, weight gain, or heart problems. In 2022, the EMA updated its guidelines to require tighter bioequivalence limits (90%-111%) for this drug class-not because the standard 80%-125% was wrong, but because the consequences of even small differences are too high.
That’s why regulators don’t let you skip one. If a generic passes AUC but fails Cmax, it’s rejected. Period. It’s not about being picky-it’s about safety.
The 80%-125% Rule: Where It Came From and Why It Works
Every generic drug submission must show that the ratio of its Cmax and AUC to the brand-name drug falls between 80% and 125%. That means the generic’s values can’t be more than 20% lower or 25% higher than the original. This range isn’t arbitrary. It’s based on decades of clinical data and statistical modeling.
In the early 1990s, regulators analyzed thousands of drug studies and found that differences beyond this range were consistently linked to changes in effectiveness or side effects. Below 80%, patients often didn’t get enough drug. Above 125%, toxicity risks rose. The 80%-125% window became the global standard because it’s the point where clinical outcomes stay stable across most drugs.
Here’s how it works in practice: if the brand-name drug has an AUC of 100 mg·h/L, the generic must fall between 80 and 125 mg·h/L. The same applies to Cmax. But here’s the catch-these numbers aren’t averaged. They’re calculated using the geometric mean of all participants’ results, and the 90% confidence interval must fall entirely within 80%-125%. This isn’t just a point estimate-it’s a statistical guarantee.
Why geometric mean? Because drug concentrations in blood don’t follow a normal bell curve-they follow a log-normal distribution. That means a few high readings can skew the average. Logarithmic transformation fixes this, and regulators require it. Most labs now use software like Phoenix WinNonlin to handle these calculations automatically.
How Bioequivalence Studies Are Done
These aren’t simple tests. A typical bioequivalence study involves 24 to 36 healthy volunteers. Each person takes both the brand-name and generic versions-sometimes in different orders, sometimes with a washout period in between. This is called a crossover design, and it removes individual differences in metabolism from the equation.
Blood samples are drawn every 15 to 30 minutes in the first few hours, then less frequently as the drug clears. For fast-absorbing drugs like aspirin, sampling might happen every 10 minutes during the first hour to catch the true Cmax. Missing even one key time point can throw off the whole result. In fact, studies show that 15% of failed bioequivalence tests are due to poor sampling timing.
Modern labs use liquid chromatography-tandem mass spectrometry (LC-MS/MS) to detect drug levels as low as 0.1 nanograms per milliliter. That’s like finding a single drop of water in an Olympic swimming pool. These tools make it possible to test even tiny doses accurately.
Once the data is collected, it’s analyzed using strict statistical methods. The FDA and EMA require that both AUC and Cmax pass independently. One failing means the entire application is rejected. No exceptions.
When the Rules Get More Complex
Not all drugs play by the same rules. For drugs with high variability-where one person’s body absorbs it way differently than another’s-the standard 80%-125% range can be too strict. Take cyclosporine, an immunosuppressant. Its absorption can vary by 40% or more between people, even when taking the same dose. If you forced it to meet the standard, no generic would ever pass.
That’s why the EMA and FDA allow something called reference-scaled average bioequivalence. It’s a special adjustment: the acceptable range widens based on how variable the original drug is. But this isn’t automatic. Companies must prove the drug’s variability is truly high, and regulators review every case individually.
For modified-release pills-those that release drug slowly over 12 or 24 hours-the picture gets even trickier. A single AUC and Cmax might not capture multiple peaks in absorption. That’s why the FDA is now exploring partial AUC measurements (like AUC from 0 to 8 hours) for these drugs. The goal? To make sure the drug releases the right amount at the right time, not just that the total exposure is close.

Why This All Matters to You
Every year, over 1,200 generic drugs get approved in the U.S. alone. That’s billions of pills taken by real people-your parents, your friends, maybe you. And every single one had to pass the Cmax and AUC test.
Research from JAMA Internal Medicine reviewed 42 studies comparing generics and brand-name drugs. The conclusion? No meaningful difference in safety or effectiveness-when bioequivalence criteria were met. That’s not luck. It’s science.
But it’s also why you should never switch generics without checking with your pharmacist. Different manufacturers use different fillers, coatings, and manufacturing methods. Even small changes can affect how fast the drug dissolves. That’s why Cmax can vary-even if AUC stays the same.
So when you see a cheaper pill on the shelf, know this: it didn’t just get approved because it looks the same. It went through a rigorous, science-backed process. And Cmax and AUC were the gatekeepers.
What’s Next for Bioequivalence?
Will Cmax and AUC always be the gold standard? Probably. Even as new tools like computer modeling and AI emerge, regulators still trust these two metrics. Why? Because they’ve been tested for over 40 years. They’re reliable, measurable, and directly tied to how drugs work in the body.
But the future might add layers. For example, researchers are now looking at how gut bacteria affect drug absorption, or how food changes Cmax in real time. These won’t replace AUC and Cmax-they’ll just help explain why they vary from person to person.
For now, the system works. It’s simple, transparent, and backed by hard data. And for the millions who rely on affordable medicines, that’s what matters most.
What does Cmax stand for in bioequivalence?
Cmax stands for maximum plasma concentration-the highest level a drug reaches in your bloodstream after taking it. It tells you how quickly the drug is absorbed and is especially important for drugs where peak levels affect how well they work or how likely they are to cause side effects.
What does AUC mean in pharmacokinetics?
AUC stands for area under the curve. It measures the total amount of drug your body is exposed to over time, from when you take the pill until it’s completely cleared. It reflects the overall exposure and is critical for drugs that need to stay in your system for hours, like antibiotics or blood pressure medications.
Why do regulators require both Cmax and AUC to prove bioequivalence?
Because they measure different things. Cmax shows how fast the drug enters your blood-important for drugs that need a quick peak, like painkillers. AUC shows how much total drug you get over time-critical for drugs that need sustained levels, like antidepressants. If only one matches, the drug might work differently in your body, even if the other value looks good.
What is the 80%-125% rule in bioequivalence?
It’s the acceptable range for the ratio of generic to brand-name drug values. The 90% confidence interval for both Cmax and AUC must fall entirely between 80% and 125%. This means the generic can’t be more than 20% lower or 25% higher than the original. This range was established based on decades of clinical data showing that differences beyond this point can affect safety or effectiveness.
Are generic drugs really as safe as brand-name ones?
Yes-if they pass bioequivalence testing. A 2019 meta-analysis of 42 studies found no meaningful difference in safety or effectiveness between generic and brand-name drugs that met the Cmax and AUC standards. Regulatory agencies like the FDA and EMA require strict testing before approval. The system works because it’s based on real pharmacokinetic data, not just appearance or cost.




Amy Insalaco
January 31, 2026 AT 00:21The entire Cmax/AUC paradigm is a statistical mirage engineered by regulatory capture. You think the 80%-125% range is grounded in clinical reality? It’s a relic from the 1990s, based on flawed log-normal assumptions and underpowered studies with n=24. Modern pharmacometrics has moved on-population PK/PD modeling, machine learning-based absorption profiles, and real-world exposure mapping have rendered these crude metrics obsolete. Yet the FDA clings to them like a religious text because changing the standard would invalidate decades of regulatory precedent-and expose the fact that 30% of approved generics have clinically significant pharmacokinetic divergence masked by geometric mean averaging. The real scandal? They don’t even require bioequivalence testing for prodrugs where active metabolites matter more than parent compound kinetics. You’re being sold a myth wrapped in p-values.
kate jones
January 31, 2026 AT 02:07It’s important to recognize that the bioequivalence framework isn’t perfect, but it’s the most rigorously validated system we have. The 80%-125% range was established after analyzing over 12,000 drug comparisons across multiple therapeutic classes, and it consistently correlates with clinical outcomes. The use of geometric means and log-transformation isn’t arbitrary-it’s mathematically necessary given the log-normal distribution of plasma concentrations. Modern LC-MS/MS methods allow detection at sub-nanogram levels, ensuring even minor differences are captured. Regulatory agencies don’t approve generics lightly; each submission undergoes multiple layers of statistical and clinical review. The fact that generic drugs account for over 90% of prescriptions in the U.S. without a spike in adverse events speaks volumes about the system’s reliability.
Rob Webber
February 1, 2026 AT 02:49Stop lying to the public. The FDA approves generics based on paperwork, not real-world performance. I’ve switched from brand-name Lamictal to three different generics over five years-each one gave me different side effects, different seizure thresholds, different moods. My neurologist says ‘they’re bioequivalent,’ but my brain knows better. Cmax and AUC are lab fantasies. Real people aren’t healthy volunteers in a controlled crossover trial. We’re eating different food, taking other meds, sleeping poorly, stressed out. The system is designed to protect Big Pharma’s profits, not patients. And now they’re pushing AI to ‘optimize’ the math so they can approve even shittier generics. Wake up.
Yanaton Whittaker
February 2, 2026 AT 06:27USA invented this system. Europe copied it. China and India are now trying to fake it. You think some guy in Mumbai is running LC-MS/MS with the same precision as a FDA-certified lab in Maryland? Nah. The 80%-125% rule is a joke when 60% of generic manufacturers don’t even have proper QA protocols. I’ve seen the reports-batch inconsistencies, fillers that alter dissolution rates, capsules that don’t even break down in the gut. And yet they get approved because the FDA is understaffed and overworked. Don’t be fooled. This isn’t science-it’s a global scam where American patients pay for cheap pills made in countries with zero accountability. If you want real safety, buy brand. Otherwise, you’re gambling with your life.
Kathleen Riley
February 4, 2026 AT 05:21One is compelled to observe that the regulatory architecture governing bioequivalence constitutes a paradigm of epistemological rigor, wherein empirical observation is subordinated to statistical inference in service of public health. The geometric mean, as a central tendency measure under log-normal distributions, serves not merely as a computational artifact but as a philosophical anchor-reflecting the inherent heteroscedasticity of pharmacokinetic phenomena. The insistence upon dual parameters-Cmax and AUC-demonstrates a profound ontological commitment to the multidimensionality of drug exposure, resisting the reductive temptation to conflate temporal kinetics with cumulative dosage. One must therefore regard the 80%-125% interval not as an arbitrary threshold, but as a transcendental boundary, derived from the convergence of clinical epistemology and mathematical necessity.
Beth Cooper
February 5, 2026 AT 11:20Did you know the FDA used to test generics on prisoners in the 80s? That’s why they trust Cmax so much-it was originally measured on inmates who were given placebos and told it was the real thing. The whole bioequivalence system is a cover-up for corporate collusion. Big Pharma owns the labs, owns the software (Phoenix WinNonlin is just a front for Pfizer’s data manipulation tools), and the ‘healthy volunteers’? Mostly paid college kids who lie about their meds. And the 80%-125% rule? That’s not science-that’s a loophole. The real reason they don’t change it is because if they did, they’d have to admit that 1 in 5 generics are dangerous. They’d rather keep you blind than lose profits. I’ve got documents. Want to see them?
Gaurav Meena
February 6, 2026 AT 07:17As someone from India where generics save lives daily, I want to say this: the system works because it’s grounded in science, not fear. I’ve worked with pharmacists who’ve seen patients switch from $300 brand-name insulin to $10 generics-and live normal lives. Yes, there are bad actors, but the regulators are improving. The EMA’s tighter limits for levothyroxine? That’s progress. LC-MS/MS is now standard in even small labs here. And the real win? Millions of people who couldn’t afford meds before now can. Don’t let fear of outliers blind you to the scale of good this system does. Keep asking questions-but don’t throw out the baby with the bathwater.
Katie and Nathan Milburn
February 7, 2026 AT 21:00Interesting read. I’m a data analyst in pharma R&D. The statistical methods described here are textbook correct-log-transformation, geometric means, 90% CI constraints. But what’s rarely discussed is the human variability behind the numbers. Two people can take the same pill, have identical Cmax and AUC, but one metabolizes it through CYP3A4 and the other through UGT2B7-leading to wildly different clinical effects. The current system assumes homogeneity, but biology is messy. Maybe the future isn’t tighter thresholds, but personalized bioequivalence thresholds based on pharmacogenomics. We’re already seeing this in oncology. Could be the next evolution.