What Happens During an FDA Inspection of a Generic Drug Facility?
When the FDA shows up at your generic drug manufacturing plant, it’s not a surprise visit meant to catch you off guard-it’s a routine check to make sure you’re producing medicine that’s safe, effective, and consistent. The agency doesn’t just walk in and start asking questions. They come with a plan, a checklist, and years of experience tracking exactly what goes wrong-and what goes right-in drug production.
The inspection is built around the Current Good Manufacturing Practices (CGMP), or 21 CFR Part 211. These aren’t suggestions. They’re legal requirements. Every step of making a generic pill-from the raw chemicals to the final box-must follow strict rules. The FDA uses a 6-system approach to evaluate your facility: Quality, Facilities & Equipment, Materials, Production, Packaging & Labeling, and Laboratory Control. And here’s the key: Quality is always reviewed, no matter what. If your quality unit isn’t independent, empowered, and active, the rest of your operation is at risk.
Types of Inspections You Might Face
Not all FDA inspections are the same. There are four main types, and which one hits your door depends on your situation.
- Pre-Approval Inspection (PAI): This happens before the FDA approves your generic drug. They’re not just checking if you can make the pill-they’re verifying that everything in your application matches what’s happening on the floor. Is the equipment you listed actually installed? Are your analytical methods the same as what you submitted? Are stability samples stored at the right temperature? If there’s a mismatch, your approval stalls.
- Routine Surveillance Inspection: These happen every 1-3 years, based on risk. A facility with a clean record and low-risk products might go longer between visits. A site with past issues, high-volume production, or complex formulations gets checked more often. The FDA uses a risk-based model that considers complaints, past findings, and even tips from insiders.
- For-Cause Inspection: Triggered by something specific-a consumer complaint, a contaminated batch, a whistleblower report. These are intense. Investigators zero in on the problem area but still look at the whole system. Don’t assume they’ll only check the one thing you think they’re after.
- Follow-Up Inspection: After you get a warning letter or an FDA 483, they come back to see if you fixed it. And they’ll check if your fixes actually work.
What the FDA Looks For-The Real Details
It’s not enough to have SOPs on a shelf. The FDA wants to see proof that those procedures are followed every day. Here’s what they dig into:
- Data Integrity: Are your lab records real? Are electronic logs tamper-proof? Are stability data points deleted or altered? Investigators check for backdated entries, unexplained outliers, and handwritten notes that don’t match instrument prints.
- Process Validation: Can you prove your manufacturing process consistently makes the same product? They’ll ask for batch records from the last 10-20 batches. They’ll check if your acceptance criteria match your validation protocol.
- Equipment Qualification: Did you test your mixers, fillers, and ovens before using them? Do you have calibration logs? Are maintenance records complete? If you can’t show that your equipment is qualified and maintained, your entire production line is suspect.
- Supplier Qualification: Where do your active ingredients come from? Did you audit your supplier? Do you have certificates of analysis for every batch? If your raw material is bad, your pill is bad-even if you did everything else right.
- Quality Unit Authority: 21 CFR 211.22(a) is one of the most common violations. The quality unit must have the power to stop production. If your production manager overrides a quality rejection, that’s a red flag.

What Is an FDA 483-and Why It Matters
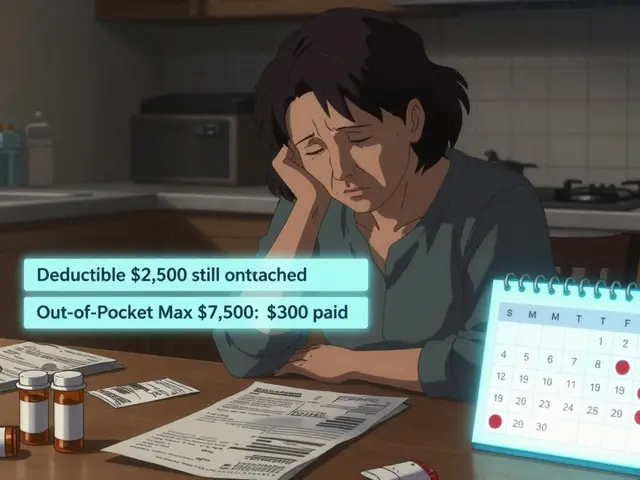
If the inspectors find problems, they’ll hand you an Form FDA 483. This isn’t a citation. It’s a list of observations-usually 5 to 15 items-ranked by severity. Each one references a specific regulation, like 21 CFR 211.110 for inadequate testing or 21 CFR 211.194 for poor record retention.
You have 15 business days to respond. This is your chance to explain, not just apologize. A good response includes:
- Root cause analysis-why did this happen?
- Corrective actions-what did you fix?
- Preventive actions-how will you stop it from happening again?
- Timeline-when will each step be done?
Don’t ignore the 483. If your response is weak, the FDA may issue a warning letter. That’s a public document. It can block your product approvals, scare off customers, and trigger more inspections.
How to Prepare-Beyond the Checklist
Most companies prepare for weeks before an inspection. That’s too late. The best facilities operate in a permanent state of readiness. Here’s how:
- Run mock inspections. Bring in a consultant or an ex-FDA inspector. Let them walk through your plant with a clipboard. Record the questions. Fix the gaps.
- Keep your facility clean and organized. Cluttered storage, dirty equipment, and unlabeled containers scream “lack of control.” Even if it’s not a violation, it makes inspectors nervous.
- Train your staff. The FDA talks to everyone-from the lab tech to the janitor. If someone says, “I don’t know why we do it this way,” that’s a problem.
- Use the PreCheck program. Launched in 2024, this is your chance to get FDA feedback before you even build your facility. Submit a Type V Drug Master File (DMF) with your layout, quality system, and validation plans. The FDA reviews it and tells you what’s missing. It’s free, and it saves millions in rework.

What Happens After the Inspection
The inspection ends with an Establishment Inspection Report (EIR). This is the official record. It includes:
- What systems were reviewed
- What was observed
- Whether the facility was in a “state of control”
- Any deviations from CGMP
The FDA classifies the outcome as either acceptable or unacceptable. If it’s acceptable, you’re good to go. If it’s unacceptable, you’ll get a warning letter. And if you ignore it? The FDA can refuse to approve your drug, seize your product, or even shut you down.
But here’s the good news: over 90% of inspections find acceptable compliance. The system works when companies take quality seriously-not as a cost center, but as the foundation of their business.
The Bigger Picture: Why This Matters for Patients
Generic drugs make up 90% of prescriptions in the U.S. They’re cheaper, but they’re not second-rate. The FDA’s inspection system ensures that a generic pill made in India, China, or Ohio delivers the same result as the brand-name version. A single failure-contaminated active ingredient, incorrect dosage, unstable product-can hurt patients. That’s why the FDA doesn’t just inspect for paperwork. They inspect for culture. For accountability. For the quiet commitment of people who show up every day and do the right thing, even when no one’s watching.
What’s New in 2025
The FDA’s approach keeps evolving. In June 2025, they finalized guidance on Post-Warning Letter Meetings (PWLMs). This gives companies a formal chance to sit down with FDA officials after a warning letter, explain their corrective actions, and get direct feedback. It’s not a loophole-it’s a lifeline. It shows the FDA wants to help compliant companies fix problems, not just punish them.
Also, the PreCheck program is expanding. More manufacturers are using it to avoid costly mistakes before they happen. The message is clear: the FDA wants you to succeed-if you’re serious about quality.


Alyssa Torres
November 19, 2025 AT 18:23Also, PreCheck is a GAME CHANGER. We submitted our DMF last month and got feedback on 3 gaps before we even installed the mixer. Saved us $200k in rework.
Summer Joy
November 21, 2025 AT 17:00Matthew Karrs
November 22, 2025 AT 22:55Michael Fessler
November 24, 2025 AT 02:37Matthew Peters
November 25, 2025 AT 19:55Liam Strachan
November 26, 2025 AT 19:46Ron and Gill Day
November 27, 2025 AT 17:07Aruna Urban Planner
November 28, 2025 AT 07:52Nicole Ziegler
November 30, 2025 AT 01:30Gerald Cheruiyot
November 30, 2025 AT 03:34Dana Oralkhan
December 1, 2025 AT 07:33