When a mate breaks their hip just by tripping on the way to put the kettle on, it makes you stop and think for a minute. Osteoporosis is sneaky. It strikes when people least expect it and can turn a simple fall into hospital drama. That’s why doctors have prescriptions ready for something called Fosamax—one of those names you see scribbled on scripts after a bone density scan raises red flags. If you’ve just been handed a bottle of white tablets and told to take them, there’s a heap you might be wondering. Maybe you’re looking out for your parents as they age, or you’re at that stage when bone strength isn’t just a footy stat, it’s something your future self relies on. People talk about calcium, exercise, and milk, but when a script brings the word Fosamax into your pantry, it gets real.
Breaking Down Fosamax: What’s In It and Why Do Doctors Prescribe It?
Fosamax is the trade name for alendronate sodium. It belongs to a class of drugs called bisphosphonates, which basically means it works on your bones at a chemical level. Doctors reach for Fosamax to treat osteoporosis—that’s when bones become brittle and prone to breaking. This isn’t only a “woman’s problem” after menopause, by the way. Men can get osteoporosis too, though it’s often underdiagnosed in blokes. If your bone mineral density scan (usually a DEXA scan) shows your bones are thinning, especially after 50, your GP might bring up Fosamax to stop the slide.
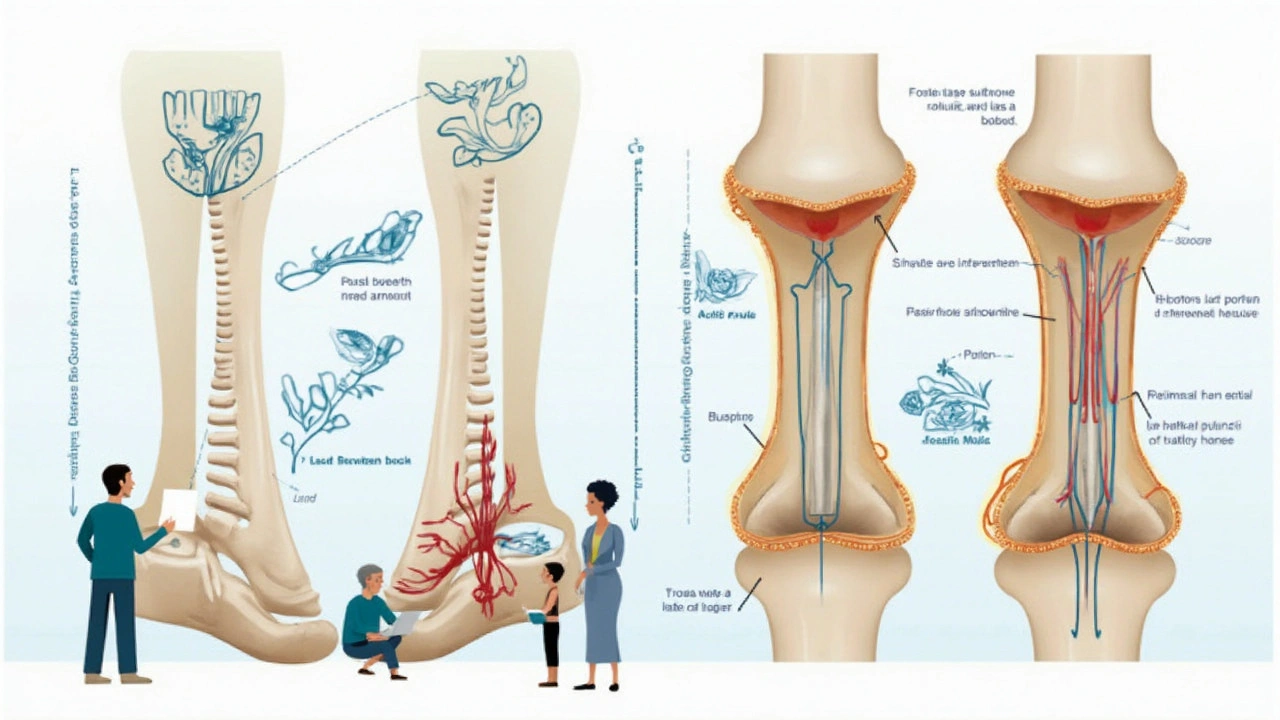
So how does it work? Your bones are in a permanent cycle of breaking down and rebuilding, even after you stop growing taller. Specialized cells called osteoclasts chew up and remove old bone, while osteoblasts build new material. As you age, the destructive crew sometimes work faster than the builders, which leads to bone loss. Fosamax blocks the action of those pesky osteoclasts. No wild chemicals, just what your system needs to rebalance bone turnover. This is important because in the real world, less bone equals higher fracture risks, which means longer hospital stays, lost independence, and plenty of headaches for families.
You’re most likely to be prescribed Fosamax if you’re in one of these groups:
- Women post-menopause with a bone density T-score of -2.5 or lower
- Men and women who have already broken a bone due to low bone density (a “fragility fracture”)
- Anyone on long-term steroids for conditions like asthma or rheumatoid arthritis, which fast-track bone loss
- People with certain cancers or medical conditions that affect hormones or nutrition
One interesting fact out of Melbourne's Royal Women's Hospital: one in three women over age 50 will have a fracture in their lifetime because of osteoporosis. That’s as common as needing a plumber in this city. That’s why doctors see Fosamax as a backbone of osteoporosis care, alongside diet and exercise.
How to Take Fosamax: The Routine, The Rules, and Common Mistakes
If you’re new to Fosamax, the way you take it matters—probably more than you think. This isn’t the average pill you chew with your morning coffee or down after a big meal. Fosamax is absorbed best on an empty stomach, but the side effect risk can creep up if you ignore the instructions. Here’s the golden rule: take it first thing in the morning, before you eat or drink anything else (except plain water). Pop the pill with a full glass of water—around 200-250mL—and stay upright for at least 30 minutes. No sneaky lie-downs, no breakfast in bed. Stand up or walk around, because if the tablet lodges in your esophagus, it can cause nasty irritation.
Food, coffee, and even some juices can stop Fosamax getting where it needs to go. If you break the routine, you’re throwing away most of the benefit. People who start with good intentions drop off after a while, letting life get in the way, or they forget the upright rule and end up with heartburn or throat pain. This is why specialist osteoporosis nurses in places like the Peter MacCallum Cancer Centre run group info sessions: it’s that easy to muck it up.
Some quick tips to keep you on track:
- Set a phone alarm for Fosamax time—you don’t want breakfast to get in the way.
- Stick the prescription on your fridge or bathroom mirror as a reminder.
- Keep a bottle of water by your bed so you can take the tablet before the morning chaos starts.
- Ask your GP about alternative forms (like weekly tablets or oral solutions) if the daily pill feels like too much of a hassle.
Kids and younger adults don’t usually take Fosamax unless they have rare bone conditions. The main players are those in the “midlife tune-up” years. Most patients use it for five years and then see their doctor about a “bisphosphonate holiday”—a pause to lower long-term risks if their bones are stable. When my dad was put on Fosamax, his GP joked it was “the closest thing to a hard hat for bones.” It stuck with him.
Benefits and Side Effects: Real Talk, Real Cases
If you listen to people who swear by Fosamax, they’ll tell you their bones haven’t let them down, even after slipping on dodgy tiles. But it’s not all smooth sailing—this medication isn’t without side effects and controversy. Most people tolerate it pretty well, especially if they follow the upright rule and stick to the schedule. The biggest benefits come down to hard stats: studies show Fosamax lowers the risk of vertebral fractures by around 50% and decreases hip fracture risk by about 30%, especially in high-risk women and men.
But there’s a flipside. Some users get stomach pain, acid reflux, or even ulcers in the esophagus if they don’t follow directions. A smaller group—less than 1%—develops jaw osteonecrosis (basically, jawbone problems), especially after dental surgery. This spooked a lot of people when it first made headlines, but dentists now recommend sorting dental work before starting Fosamax if you can. Another rare issue is “atypical femur fractures”—unusual thigh bone breaks, usually after years of use. That’s why regular check-ins and “drug holidays” make sense if you’re stable.
Then there’s the thing nobody talks about: people sometimes skip doses or stop Fosamax after a few weeks because they think they feel fine, or they read scary things online. This is one of those medications where “not feeling sick” is actually the goal—bone loss doesn’t hurt until a break happens. If you’re on Fosamax for years, it helps to have a doctor who’ll check in, keep tabs on blood calcium and vitamin D, and revise your plan as you age.
Here’s a solid reminder from Professor Peter Ebeling, head of endocrinology at Monash University:
"Fosamax and related drugs are still the single most effective option for preventing fractures in people with osteoporosis. Taking them correctly is what counts—most side effects can be avoided by following simple instructions and discussing your concerns with your GP."That’s from someone who’s seen thousands of bone scans and hospital stays turned around by a little white pill and a good routine.
If you ever start the med and notice chest pain, swallowing problems, or jaw pain, don’t brush it off—call your doctor right away. They can usually sort things quickly, but you’re better off safe than sorry.
Maximizing Bone Health: Beyond Fosamax, The Real-World Plan
Medication isn’t a magic bullet—you need to back it up with some old-fashioned healthy habits. Vitamin D, calcium-rich foods, and weight-bearing exercise matter more than any single pill. Even in sunny Melbourne, vitamin D levels dip fast in winter or for people who cover up or stay indoors. That’s why regular blood tests are a must. Dairy’s great, but if you’re lactose intolerant or vegan, stock up on alternatives like calcium-fortified plant milks, green leafy veg, and tinned sardines or salmon (bones in, if you can stomach them!)
Weight-bearing exercise like walking, dancing, or strength training tells your bones to hang on to calcium and stay strong. You don’t need a gym membership—carrying heavy shopping bags or gardening count, too. If you’ve already broken a bone, you’ll probably get a tailored program from a physio to build core muscle and balance. Staying active makes a big difference: studies from the University of Queensland found that regular brisk walking lowered the risk of falls by building up leg strength and bone density in women over 60.
Another sneaky culprit in bone loss is smokes and heavy drinking. Both chip away at bone strength over time, so quitting or cutting down can pay dividends. If you’re on other meds that mess with bones—things like steroids, epilepsy drugs, or certain cancer therapies—remind your doctor every few months to keep an eye on your bone health.
Tracking your progress: Every patient’s journey is a bit different. After starting Fosamax, most GPs or specialists will repeat bone density scans every two to three years. If your score is stable or improving, you might get a break from the medication. If it’s going backwards or you have new fractures, the doctor might try a different medication. Family history matters too. If your parents or siblings have had hip fractures, stay proactive. Chat to your doctor about their experience and what extra screening you might need.
Finally, don’t underestimate how a supportive home or community can keep bones safe. Simple fixes—good lighting, non-slip mats, removing trip hazards—can stop the sort of falls that send you to hospital. If you have older relatives, or you’re heading for retirement yourself, think about tweaking your house now. You’ll thank yourself later.
So whether you’re picking up your first blister pack of Fosamax or managing it for a loved one, stick with the plan. Take it right, eat well, move more, and keep the convo going with your GP. Protecting your bones isn’t just about now—it’s your ticket to staying on your feet and living the good life for years to come.


fred warner
July 18, 2025 AT 04:48Really insightful post about Fosamax and its importance for combating osteoporosis, especially in Australia where aging populations are quite significant. I appreciate the clear explanation of how Fosamax works and the emphasis on both the benefits and side effects. Often, people just see medication as a quick fix, but this article encourages a mindful approach to bone health.
One point I found particularly noteworthy was the detailed discussion on who should take Fosamax. Tailoring treatments like this avoids unnecessary risks and enhances effectiveness. Definitely something to share with family or friends who might be considering this.
Does anyone have experience balancing lifestyle changes along with this medication? It’d be interesting to hear thoughts on diet and exercise supplements to Fosamax use.
Veronica Mayfair
July 20, 2025 AT 01:15Oh wow, this article really nails it! 🙌 I love how it dives into both the science and real experiences. It’s so important for folks to understand what they're taking, you know? Sometimes meds can be super intimidating.
Side effects are always scary, but it’s reassuring to see them addressed so honestly here. Plus, the tips for making treatment work better – like timing your dose or what to avoid eating right after – are golden! 🌟
Anyone here tried Fosamax? How did you feel after starting treatment? Please share your stories, more than happy to swap experiences. 🙂
Rahul Kr
July 21, 2025 AT 21:41Thanks for the detailed explanation. Osteoporosis is a silent condition, so it's good to see detailed info about a medication like Fosamax that can help.
From what I've read, it's crucial not just to rely on meds but also to ensure adequate calcium and vitamin D intake. The article touches on nutrition but could maybe dive deeper into how these elements support Fosamax's effectiveness. 🤔
And the risks versus benefits discussion is important—it’s always a balance. Interesting read overall, thanks for sharing!
Sarah DeMaranville
July 23, 2025 AT 18:08Seriously, Fosamax. The trend of jumping onto pharmaceutical bandwagons without proper scrutiny is disconcerting.
I doubt the average patient is given enough understanding of the trade-offs involved. The article mildly touches on side effects but conveniently omits the controversial cases emerging in recent literature. Osteoporosis isn’t solved by a pill alone.
Maybe focus should shift more to lifestyle, diet, and exercise rather than blindly ingesting meds promoted as a cure-all. Just saying.
Edward Leger
July 25, 2025 AT 14:35It's fascinating how medication like Fosamax intersects with the philosophical notions of health and aging. The article implicitly raises questions about the human desire to stave off natural decline and how medical interventions both answer and complicate these desires.
Is it not also an opportunity to reconsider how we value vitality versus longevity? The bone is but one metaphor for our fragile existence.
In that sense, Fosamax represents more than a drug; it embodies the tension between acceptance and resistance in the human condition.
Ismaeel Ishaaq
July 27, 2025 AT 11:01Absolutely captivating article! The way it demystifies the workings of Fosamax is like having your own personal encyclopedia at your fingertips. I can't stress enough the importance of education in medicine; many are clueless about their treatments' actual impact.
That said, I do yearn for more patient testimonials here. Real stories add vibrant hues to clinical facts, and I believe they were touched upon but could be amplified. Knowledge is power, but shared experiences spark inspiration!
Jesse Goodman
July 29, 2025 AT 07:28Good article. Fosamax does help bones stay strong. Simple facts, no fluff.
Side effects are there, so careful. People should talk to their doctors first. Also, not just pills matter, diet and activity important too.
That’s all. Hope it helps.
🙂Antara Kumar
July 31, 2025 AT 03:55Honestly, while this might be relevant for Australia, let’s not pretend it applies universally. Osteoporosis treatment varies greatly between nations, and taking a drug like Fosamax without proper context is irresponsible.
The article lacks any critique of the pharmaceutical influence on treatment guidelines. Why do Australians prefer Fosamax so much? Could this be pushed by vested interests? These are the questions I'd rather see addressed.
John Barton
August 2, 2025 AT 00:21Oh great, another 'miracle' pill touted for aging bones. How novel. So is this the stuff that turns fragile oldies into superhero statues overnight or what? I'm skeptical, not to mention side effects lurking like creepy villains.
But seriously, folks, any meds need careful inspection, not just hopping on the hype train. Does anyone here have real-deal results or stories beyond the glossy sales pitch?
Achint Patel
August 3, 2025 AT 20:48Interesting read. I wonder about the accessibility of Fosamax in rural areas though, especially in places with less healthcare infrastructure. The article doesn't cover that aspect.
Moreover, discussions on dosage timing and interactions with other treatments could be expanded. Sometimes these details make all the difference in success.
Would be great if the author weighs in on these points.
Lilly Merrill
August 5, 2025 AT 14:28I appreciate the calm tone and thoroughness here. Discussing osteoporosis with nuance helps remove stigma about aging and bone fragility. The inclusion of tips to maximize the benefits of Fosamax is practical and user-friendly.
That said, I resonate with others about wanting more firsthand patient stories. Learning from lived experiences can create a supportive community around health challenges.
Thanks for sharing such a balanced article!