Medications can be life-changing, sometimes for all the wrong reasons. Imagine popping a pill for high blood pressure and waking up the next morning with lips twice their normal size or feeling your throat start to tighten. That’s angioedema in action—and it happens more than people think. While not every medicine causes this, some do, and the effects can sneak up on you out of nowhere—even after months with no problems at all.
A lot of people never hear about angioedema until it hits them, so being aware can literally be the difference between a close call and something dangerous. You don’t need a medical degree to spot the signs. Swelling around the mouth, eyes, hands, or even your stomach can mean you’re having a reaction to your medicine. A red, itchy rash isn’t always part of the picture—sometimes, it’s just the swelling.
Knowing which meds are most likely to cause angioedema, and what to do if something feels off, could save a tense trip to the ER (or a scarier outcome). If you’ve got a prescription—especially for things like ACE inhibitors for blood pressure, NSAIDs for pain, or certain antibiotics—keep an eye on new swelling and tell your doctor fast if anything changes. Your body likes to give warning signs. Trust them.
- What is Angioedema and Why Do Medications Matter?
- Common Medications Linked to Angioedema
- How to Recognize a Medication Reaction Fast
- What To Do If You’re at Risk (or Reacting)
What is Angioedema and Why Do Medications Matter?
Angioedema looks simple on paper—it’s sudden swelling that can show up almost anywhere on the body, but most often hits the face, lips, tongue, throat, or even your gut. It's scary because it can make breathing difficult if the throat swells, and it’s way more common than people realize. The tricky part? It isn’t always itchy and doesn’t always come with hives, so it’s easy to miss at first.
So, what’s actually happening? With angioedema, tiny blood vessels leak fluid into nearby tissues, causing those areas to puff up. The cause can range from allergies, genetics, or even just stress. But here’s the kicker: medication triggers are a sneaky, underreported reason for these sudden symptoms. Sometimes, you might have been on the same med for years before angioedema shows up out of the blue.
Medications matter big-time because some drugs are much more likely to trigger angioedema than others. ACE inhibitors—commonly used for high blood pressure—are one of the biggest culprits. Studies in the US show ACE inhibitors cause up to 30% of drug-induced angioedema hospital visits. It can also happen with NSAIDs (like ibuprofen), antibiotics, and even some diabetes meds.
| Drug Type | Reported Angioedema Cases (Estimate) |
|---|---|
| ACE Inhibitors | Up to 30% of drug-related cases |
| NSAIDs | Second most common |
| Antibiotics (like penicillin) | Less common, but still significant |
If you or someone you know starts a new medication, watch for any new swelling or odd sensations. Careful tracking can help spot problems early. Remember, even if you’ve never had an allergy before, you can still react to a medication trigger—sometimes, your immune system just decides it’s had enough.
Common Medications Linked to Angioedema
If you or someone close to you is suddenly dealing with weird, puffy swelling, medications should be on your radar. Certain prescriptions are notorious for being angioedema triggers. The biggest offenders? ACE inhibitors. These are super common for treating high blood pressure. It’s wild, but about 1 out of 200 people on these meds will get angioedema at some point, and it can crop up even years after starting the drug.
Let’s break down the main culprits:
- ACE inhibitors (like lisinopril, enalapril, ramipril): The most famous group, especially for swelling around the face, lips, or tongue. They don’t always cause itching, so swelling can sneak up on people.
- ARBs (angiotensin receptor blockers—losartan, valsartan): Less risky than ACE inhibitors, but still on the list.
- NSAIDs (ibuprofen, naproxen): These painkillers are everywhere, but they can definitely spark angioedema—more often in folks with a history of allergies.
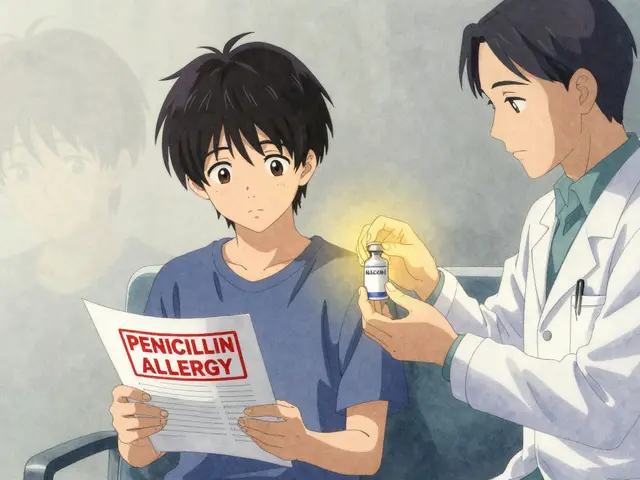
- Antibiotics (penicillins, sulfa drugs): When people report swelling and trouble breathing after antibiotics, doctors pay extra attention. Not every swelling reaction is a true allergy, but it always needs quick action.
- Contrast dyes for CT scans or MRIs: Not a daily issue, but angioedema can show up here too, usually right after the test.
Here’s a handy look at the most common medication triggers and their usual risk levels:
| Medication Type | Usual Trigger Rate |
|---|---|
| ACE inhibitors | About 0.5% |
| ARBs | Much lower, rare |
| NSAIDs | Up to 0.3% among regular users |
| Antibiotics | Rare, but serious when it hits |
| Contrast dyes | Very rare, but immediate risk |
When it comes to these angioedema triggers, always keep an eye out—especially if you’re starting a new prescription or mixing different meds. If you’ve had swelling before, tell every doctor and pharmacist right up front. They can usually find options less likely to set off a reaction.

How to Recognize a Medication Reaction Fast
When it comes to angioedema, the clock really matters. The earlier you catch the signs of a reaction triggered by medication, the better your chances are of avoiding a severe outcome. So what should you watch out for?
- Swelling: Most cases start around the lips, eyes, tongue, or even hands and feet. Sometimes swelling shows up in your stomach, causing belly pain or nausea without much visible change.
- Tightness or Trouble Breathing: If your throat feels tight, your voice changes, or you’re suddenly struggling to breathe or swallow, you need help right away. Don’t wait—these are emergency signs.
- No Rash Needed: Unlike regular allergic reactions, angioedema caused by drug allergies might not include itching or hives. The absence of a rash does NOT mean you’re in the clear.
- Onset Can Be Sudden or Delayed: Some people react within hours of taking their medication. Others might not notice symptoms until days or even weeks later, especially with ACE inhibitors.
Doctors at the Mayo Clinic say:
"Medications such as ACE inhibitors may cause angioedema even after you’ve been taking them without problems for months or even years. Never ignore new swelling or breathing changes."
If you have these symptoms while on a new—or even a not-so-new—prescription, assume it’s related and reach out to your doctor. Never assume you’re ‘overreacting’. Stats show that around 30% of angioedema cases seen in emergency departments are drug-induced.
| Common Areas Affected | Associated Symptoms |
|---|---|
| Face (lips, eyes, tongue) | Swelling, numbness, trouble speaking |
| Throat | Voice changes, trouble breathing, swallowing difficulty |
| Hands/Feet | Swelling, stiffness |
| Abdomen | Pain, nausea, vomiting |
Set up a reminder on your phone after starting a new medication—sometimes the changes are so gradual you might ignore them until they’re a real problem. If your lips or face look puffy or you feel off, play it safe and call your doctor or visit urgent care. It’s always better to check than miss a serious reaction.
What To Do If You’re at Risk (or Reacting)
If you know you’re at risk for angioedema because of meds, the best move is to plan ahead. Don’t just hope for the best—set yourself up to handle a reaction calmly and quickly.
First, talk to your doctor before starting any new prescription, especially if you’ve had swelling or allergies before. Make sure they know your full history. Sometimes, just switching away from triggers like ACE inhibitors or certain NSAIDs can lower your risk.
- Ask if there are safer medication options for you.
- If you notice swelling, stop the suspected drug immediately unless your doctor tells you otherwise. Don’t wait for it to go away on its own—angioedema can turn serious fast.
- Always keep emergency numbers handy. If your tongue, face, or throat starts swelling, call 911 or your local emergency right away. These cases can block airways, and seconds matter.
- If you’ve had a reaction before, talk to your doctor about carrying an epinephrine autoinjector (like an EpiPen)—sometimes this can buy crucial time if things get bad. Don’t assume you’re in the clear after one episode; reactions can come back even after the initial swelling goes down.
- Wear a medical alert bracelet showing your specific drug allergy or risk, so doctors and emergency services act fast if you can't speak for yourself.
People often worry about having to go off important medicines. The good news: most folks who react to one drug can find another that works just as well. For example, if you have angioedema from one blood pressure medicine, your doctor can usually choose another option.
| High-Risk Med Types | Quick Steps |
|---|---|
| ACE Inhibitors | Stop the drug, seek help, switch meds |
| NSAIDs (ibuprofen, aspirin) | Avoid, use approved alternatives |
| Antibiotics (penicillins) | Notify doctor, get allergy noted |
For daily life, snap a smartphone photo of your meds and allergies and keep it in your wallet or phone. It saves time in an emergency.
Lastly, don’t ignore your gut. If something feels wrong, even if you “think it’s nothing,” get checked out. Quick action with angioedema really matters.

Jarod Wooden
July 18, 2025 AT 04:56Ah, angioedema - the body's drama queen of allergic reactions, right? It almost feels like a biochemical betrayal when these meds suddenly decide to unleash swelling havoc. But you know, this article really sheds light on the critical nexus between pharmacology and immunology. It’s like peeling back layers of an onion, exposing how ACE inhibitors or NSAIDs might activate certain pathways, causing localized swelling that can escalate in minutes.
What gets me is the unpredictability factor — why does one person react violently while another doesn’t even twitch? It’s almost as if genetics and environment conspire coherently to determine susceptibility. Spotting early warning signs such as tingling lips or facial puffiness is not just prudent but life-saving. This it's not just about awareness—it's about mastering the art of preemptive intervention.
Bottom line: anyone dabbling with medications should cultivate a quasi-mystical vigilance. This isn’t fear-mongering; it’s informed caution in an era where self-medication is rampant. Who else here has had a close call with this?
lee charlie
July 19, 2025 AT 06:40Really appreciate this breakdown. Honestly, I've always been a bit nervous taking meds because of stories about allergic reactions. This info about angioedema triggers makes me feel more equipped to notice subtle symptoms early. Like, if I start noticing unexpected swelling or tightness, I’ll be less likely to brush it off.
Also, the article's tips on navigating prescriptions safely are reassuring. It's so easy to overlook interactions or personal risk factors. Has anyone else had a pharmacist or doctor who really helped you understand your meds better? I find those conversations super valuable.
Greg DiMedio
July 20, 2025 AT 11:50Geez, another article telling us to just "watch out" for medication side effects like angioedema. Because nobody else has ever thought of that, right? I swear, these health writes are so redundant sometimes. Like, sure swelling's bad and all, but what new groundbreaking info is here? Drugs cause side effects, surprise surprise.
Anyway, if you want the short version: ask your doc, don't be dumb, and maybe read fine print next time you swallow a pill. There, saved you five minutes of reading.
Badal Patel
July 21, 2025 AT 14:13My dear compatriots, this matter is of utmost significance. Angioedema, as highlighted, is a pernicious adversary lurking within the realm of medicinal benefactions. The tragic irony that life-affirming drugs may simultaneously harbor the capacity to suffocate vitality is a paradox worth a formal dissertation!
Permit me to emphasize — early detection is not merely advisable; it is imperative for survival. The minuscule telltale signs, often dismissed as trivial, must be scrutinized with a forensic lens. Hark to your body’s subtle alarms!
In my extensive observation, I advocate for a regimented checklist approach when initiating any new medication. Document, observe, and if necessary, retaliate by seeking immediate medical reprieve. The stakes, dear readers, are too grave for laissez-faire attitudes.
Sonia Michelle
July 22, 2025 AT 19:15This piece is so valuable because it empowers people with knowledge. Angioedema is scary, but knowing which medications commonly cause it can really help someone speak up if they notice early symptoms. Early recognition literally can be the difference between a trip to the ER and just adjusting a prescription.
I love that it also talks about practical tips—not just the scary facts but tangible advice. I’d encourage anyone reading this to have a conversation with their healthcare provider about their risk factors. It’s about partnership in health, not just blind trust.
And for those worried about past reactions, don’t hesitate to get an allergy panel or consult an immunologist. Proactive is the way.
KIRAN nadarla
July 23, 2025 AT 21:46Allow me to add, for those who presume casual attitude suffices, the gravity of monitoring angioedema triggers through medications cannot be overstated. Grammar aside, the documentation provided by physicians must be explicit. No ambiguous terminology or careless ambiguities tolerated!
The differentiation between drug-induced angioedema and hereditary forms must be clearly outlined, lest misdiagnoses proliferate. One must insist on clarity and comprehensive patient education. A mere mention of 'possible swelling' hardly suffices.
Furthermore, patient follow-ups constitute a critical component oft overlooked in practice, exposing a lacuna which, if addressed, could mitigate many adverse outcomes.
Abhimanyu Singh Rathore
July 25, 2025 AT 01:33Perfectly stated! Also, it’s high time we enhance pharmacovigilance to capture these adverse events with higher fidelity. The language in prescriptions and patient leaflets needs censorship from verbosity and tailor-made for clarity. The average patient battles not just symptoms but the linguistic labyrinths.
I posit that healthcare providers adopt a more theatrical approach in patient education - dramatization of risks to solidify remembrance. It’s about engaging the patient emotionally to ensure vigilance.
Ada Lusardi
July 26, 2025 AT 05:20Wow, all these serious points are making me realize how vital this topic really is! 😮 I once had mild swelling after a new medication, and I panicked not knowing if it would get worse. Articles like this help soothe that fear by giving practical advice and clear signs to watch for. 🙌
Also, the tips on how to discuss meds and risks with your doctor are so on point. Communication is everything in healthcare.
Thank you for breaking it down in such an approachable way! 💖
Joe V
August 1, 2025 AT 00:13While the article does well in highlighting angioedema's severity, one must question if the average patient truly absorbs this info amid complex medical jargon. The nuances of immunologic pathways are probably lost on many, reducing the practical impact.
However, I do recognize the importance of raising awareness about medication-induced risks. Perhaps a more distilled, layman-friendly approach would achieve greater penetration. After all, information is only as valuable as it is comprehended.
Doug Farley
August 3, 2025 AT 07:46Oh great, another PSA about meds being dangerous—like they’re not all basically poison when you think about it. The swelling from angioedema? Just one more reason to question modern pharmacopeia's obsession with chemicals. Sure, fine, watch for symptoms and all that jazz, but sometimes I wonder if we’re better off sticking to basics rather than these synthetic concoctions with mysterious side effects.
Anyway, nice article if you wanna keep living in fear. For me, I’ll just keep my skepticism high and my trust in Big Pharma low.
Pam Mickelson
August 16, 2025 AT 01:20This really underscores the importance of being proactive about health. I'm always advocating for patients to be their own best advocates, and knowing about potential angioedema triggers is a critical part of that.
One thing I like to remind people is to document any previous reactions carefully and share that info every time they start a new med regimen. It saves doctors and patients a lot of trouble.
Let's all commit to better communication and awareness — it truly changes outcomes.