When you’re prescribed a new medication, your doctor might say, "This works well, but some people get nausea or dizziness." That’s not enough. Side effects aren’t just statistics-they’re real, daily disruptions. One person can’t sleep because of fatigue. Another quits because of brain fog that makes their job impossible. And too often, patients don’t speak up until it’s too late. That’s where shared decision-making scripts come in. These aren’t robotic scripts. They’re structured, human conversations that help you and your doctor weigh what matters most: the benefit of treatment versus the cost to your life.
Why Talking About Side Effects Isn’t Optional
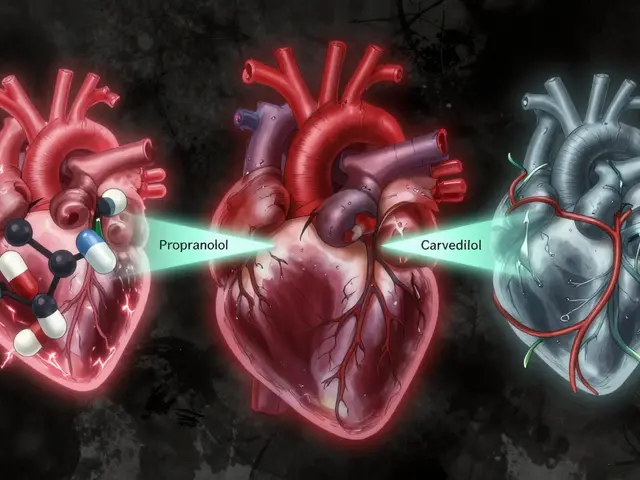
Think about statins. Eighty-six percent of people who stop taking them do so because of side effects-not because the drug didn’t work, but because the trade-off felt too high. Same with blood thinners: 3 to 5% of users face a major bleed each year. These aren’t rare. They’re common enough that every patient should know what they’re signing up for. But here’s the problem: doctors often say "rare side effects" or "mild discomfort." Those words mean nothing. One person’s "mild" is another’s nightmare. A 2021 study found that patients who got clear, numerical risk information were 37% more likely to understand what they were facing. That’s not a small gain-it’s the difference between sticking with treatment and quitting cold turkey. Shared decision-making flips the script. Instead of the doctor saying, "Take this," it becomes, "Here’s what we know. Here’s what it could cost you. What’s acceptable to you?"The SHARE Approach: A Simple Framework for Tough Conversations
The Agency for Healthcare Research and Quality (AHRQ) built a five-step model called SHARE that’s used in over 47 U.S. health systems. It’s not theory-it’s used in real clinics, every day.- Seek opportunities to include you in the decision. Your doctor should ask: "Would you like to talk about what matters most to you when choosing a treatment?"
- Help you explore options. Not just "take this pill," but "here’s option A, B, and C, including doing nothing." Each comes with different side effect risks.
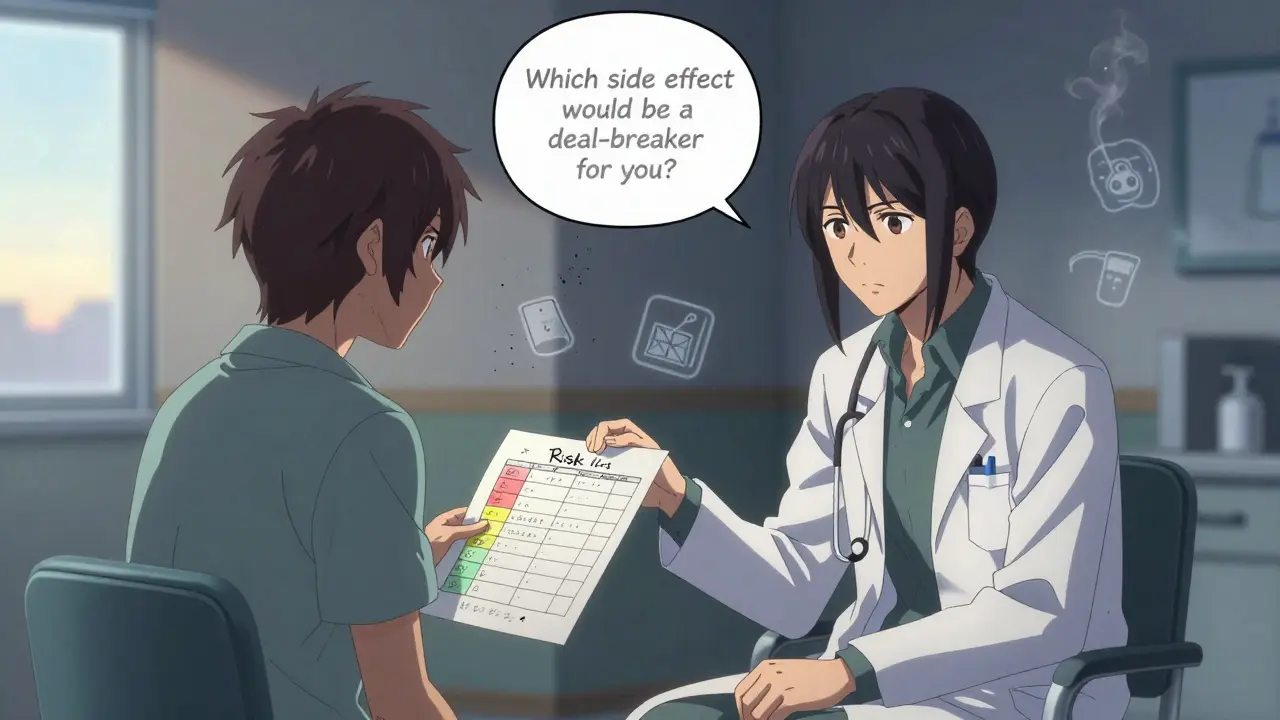
- Assess your values. This is the most important step. Instead of asking "Are you worried about side effects?" they ask: "Which side effect would make you stop this treatment?"
- Reach a decision together. Not "I think you should..." but "Based on what you’ve said, this seems like the best fit. Does that match what you want?"
- Evaluate. Later, they check in: "How’s it going? Are side effects worse than you expected?"
How to Talk About Numbers-Without Getting Lost
Doctors often say, "There’s a 50% lower risk of stroke with this drug." That sounds good. But it’s misleading. What matters is: What’s my actual risk? If your baseline risk of stroke is 2% per year, and the drug cuts that by 50%, you’re now at 1%. That’s a 1% absolute risk reduction. That’s the number you need. And it’s not "rare"-it’s 1 in 100. That’s different from saying "it reduces risk by half," which makes it sound like a miracle. The three-talk model gives clinicians a clear structure:- Option talk: "Here are your choices. Each has pros and cons."
- Decision talk: "What’s most important to you?"
- Decision support talk: "Here’s what the data says about side effects, in numbers you can use."
What Patients Really Say-And What They Wish Doctors Would Ask
On Reddit, a patient wrote: "My doctor told me my statin might cause muscle pain. I thought that meant a little soreness. Turns out, it meant I couldn’t walk up stairs. I didn’t know to say, ‘That’s not worth it.’" A 2023 survey found that 78% of patients said the single most helpful question from their doctor was: "Which side effect would be a deal-breaker for you?" That question opens the door. It says: "I’m not here to push a pill. I’m here to help you live your life." Patients also love visual tools. Color-coded charts showing risk levels-red for "high," yellow for "moderate," green for "low"-help people grasp numbers faster. Scripps Health found patient satisfaction jumped 41% when those were used. One man on HealthUnlocked said: "My doctor drew a line on a piece of paper. Said, ‘If side effects cross this line, we stop.’ That made me feel like I had control. I didn’t feel like a patient. I felt like a partner."Why This Doesn’t Always Work-And How to Fix It
Not every doctor uses this. And when they try but do it badly, it backfires. A 2022 Medscape survey found 63% of patients felt frustrated when doctors "read from a script like a robot." The problem isn’t the script. It’s the delivery. Shared decision-making fails when:- The doctor rushes through it because they’re behind schedule.
- They use jargon like "adverse event" or "comorbidity."
- They don’t listen to what the patient says after asking the question.
- They treat it like a checkbox, not a conversation.

What’s Changing Right Now
This isn’t just a nice idea. It’s becoming standard. - In 2023, Medicare Advantage plans were required to document shared decision-making for high-risk drugs like anticoagulants and diabetes meds. That means doctors are now being paid to do this right. - Epic, the biggest electronic health record system in the U.S., rolled out built-in SDM tools in 2022. Now, when a doctor prescribes a statin, the system prompts them: "Has the patient discussed side effect thresholds?" - The American Medical Association created new billing codes (96170-96171) that pay doctors $45 to $65 for documented shared decision-making sessions. And it’s not stopping. The NIH just funded $2.3 million to build AI tools that listen to doctor-patient conversations and flag when side effect concerns weren’t fully explored. That’s how seriously this is being taken.What You Can Do Today
You don’t need to wait for your doctor to bring this up. You can start it. Here’s what to say at your next appointment:- "I’ve heard this medication can cause side effects. Can you tell me which ones are most common-and which ones would make people stop taking it?"
- "What’s the chance I’ll get each one? Not ‘rare’-actual numbers."
- "Which side effect would be a deal-breaker for you if you were in my shoes?"
- "If I get side effects, what’s the plan? Do we stop, switch, or adjust?"
- "Can I get a handout or video to review this later?"
It’s Not About Perfect Decisions-It’s About Right Ones for You
There’s no perfect medication. Every drug has trade-offs. The goal isn’t to avoid side effects entirely. It’s to make sure you’re not stuck with one you didn’t expect-and that you’re not missing out on something that could help you live better. Shared decision-making isn’t about being told what to do. It’s about being heard. It’s about knowing your risk. It’s about feeling like you have a say in your own body. And that’s not just good medicine. It’s basic human respect.What if my doctor doesn’t know how to do shared decision-making?
If your doctor isn’t familiar with shared decision-making, you can still lead the conversation. Bring printed materials from trusted sources like the Agency for Healthcare Research and Quality (AHRQ) or the Informed Medical Decisions Foundation. Say, "I’ve read about this approach and would like to try it today." Many doctors will respond positively because they want to do right by patients-they just haven’t been trained to do it this way. Some clinics even have decision aids you can request before your visit.
Are side effect trade-offs only important for chronic meds?
No. While they’re most common with long-term drugs like statins, blood thinners, or antidepressants, they matter anytime a treatment has meaningful side effects. Even antibiotics can cause severe diarrhea or yeast infections. Chemotherapy drugs can cause fatigue so bad you can’t work. The key is whether the side effect impacts your daily life. If it does, it’s worth discussing-even if the treatment is short-term.
How do I know if a side effect is "normal" or something serious?
Ask your doctor to clarify: "Is this a common side effect, or does it mean something dangerous is happening?" For example, mild nausea is common with many drugs. But vomiting, blood in stool, or sudden confusion are not. Make a list of red flags before you start the medication. Keep it handy. If something matches, call immediately. Don’t wait to see if it gets better.
Can I change my mind after I’ve started the medication?
Yes. Shared decision-making isn’t a one-time contract. It’s an ongoing conversation. If side effects are worse than expected, or if your life changes (you start a new job, have a baby, or develop another health issue), you can revisit the decision. Your doctor should welcome that. In fact, follow-up discussions are part of the process. Many patients adjust their treatment plan after 4 to 6 weeks once they’ve experienced the medication.
Do these scripts work for mental health medications?
Absolutely. Antidepressants can cause weight gain, sexual side effects, or emotional numbness. Antipsychotics can cause tremors or metabolic changes. These are deeply personal trade-offs. Patients often feel ashamed to talk about them. But studies show that when doctors ask directly-"What kind of changes would you find unacceptable?"-patients are far more likely to stay on treatment and report better quality of life. Mental health care isn’t just about symptoms. It’s about living a life you want to live.


Christina Widodo
January 11, 2026 AT 12:39I love how this breaks down the real human cost of meds-not just stats. My dad stayed on a blood thinner for years because his doctor never asked what side effects he’d tolerate. He just assumed he’d "deal with it." Turns out, the brain fog made him forget his own birthday. Don’t let that happen to you.
Lawrence Jung
January 12, 2026 AT 22:55Shared decision making sounds nice but it’s just corporate medicine repackaged as empowerment. Doctors are overworked and patients are too lazy to read the leaflets. Stop romanticizing conversations that don’t scale.
Prachi Chauhan
January 14, 2026 AT 20:50My doctor once said "mild nausea" and I thought I’d just feel a little queasy. I threw up for three days straight. No one asked me what was unacceptable. They just handed me a pill and said "it gets better." It didn’t.
Katherine Carlock
January 16, 2026 AT 18:55This is exactly what I needed to hear. I’ve been too scared to ask my psych doctor about sexual side effects-felt too awkward. But now I’m going in next week with this list. Thank you for giving me the words.
Sona Chandra
January 17, 2026 AT 00:20MY DOCTOR CALLED IT "MILD FATIGUE" AND I COULDN’T GET OUT OF BED FOR A WEEK. I WASN’T ASKED WHAT I’D TOLERATE. I WAS JUST TOLD TO TAKE IT. NOW I’M DEPRESSED BECAUSE OF THE MEDS. THIS IS CRIMINAL.
Jennifer Phelps
January 17, 2026 AT 22:01I wish doctors would just show us the numbers instead of saying rare or mild. I had no idea 1 in 10 meant 10 percent. I thought it meant one person in a hospital. Not me. Not my family. Not me.
beth cordell
January 18, 2026 AT 23:48THIS CHANGED MY LIFE 🙌 I printed the SHARE framework and gave it to my cardiologist. He paused. Then said "Wow. No one’s ever done that." We spent 20 mins talking. I’m on a lower dose now and feel like myself again. You’re not a patient. You’re a person.
Lauren Warner
January 20, 2026 AT 21:37Let’s be real. This is just another way for hospitals to avoid liability. If you document that you "discussed trade-offs," you’re covered legally even if the patient didn’t understand a word. It’s performative empathy. The system isn’t broken-it’s designed this way.
Amanda Eichstaedt
January 21, 2026 AT 19:49My mom is from Mexico and didn’t speak English well. The doctor handed her a pamphlet in English and said "read this." She took the pill anyway because she didn’t want to seem difficult. Shared decision-making only works if you’re fluent in English, educated, and confident enough to push back. For most people? It’s a luxury.
Alex Fortwengler
January 22, 2026 AT 23:58Big Pharma loves this stuff. More paperwork means more billing codes. More codes means more profit. Meanwhile, patients are still getting prescribed drugs with side effects that ruin lives. This isn’t patient empowerment-it’s profit laundering dressed up as empathy.
jordan shiyangeni
January 24, 2026 AT 16:59It’s not just about the script-it’s about the entire medical-industrial complex that treats human beings as data points. The system incentivizes speed over substance, volume over validity. You can’t fix a broken paradigm with a five-step checklist. You need to dismantle the entire structure that reduces human suffering to a billing code and a checkbox. This is not medicine-it’s logistics with a stethoscope.
Abner San Diego
January 25, 2026 AT 15:58USA medical system is a joke. My cousin in Germany got a 45-minute consultation with a doctor who drew diagrams and asked what he cared about. Here? 8 minutes. "Take this. Call if it gets worse." That’s not care. That’s corporate triage. And now they’re paying doctors to pretend they care? Pathetic.
Sumit Sharma
January 27, 2026 AT 08:29The SHARE framework is clinically validated and endorsed by AHRQ-this isn’t opinion, it’s evidence-based practice. Your resistance to structured communication is precisely why patients suffer. If you can’t articulate risk numerically, you’re not a clinician-you’re a gatekeeper. The data is clear: patients who understand their trade-offs have better adherence, lower regret, and fewer ER visits. Stop pretending intuition trumps transparency.
Cecelia Alta
January 28, 2026 AT 20:57Look, I get it. People want to feel heard. But let’s not pretend this is revolutionary. I’ve been in clinics for 15 years. Every doctor says they do shared decision-making. But when the clock hits 10:30 and the next patient is waiting? They skip the "deal-breaker" question and hand out the script. This is performative. The system doesn’t change because you give patients a handout. It changes when you pay doctors to listen. And we’re still not doing that.