Antiplatelet Effects: How Blood Thinners Work and What You Need to Know
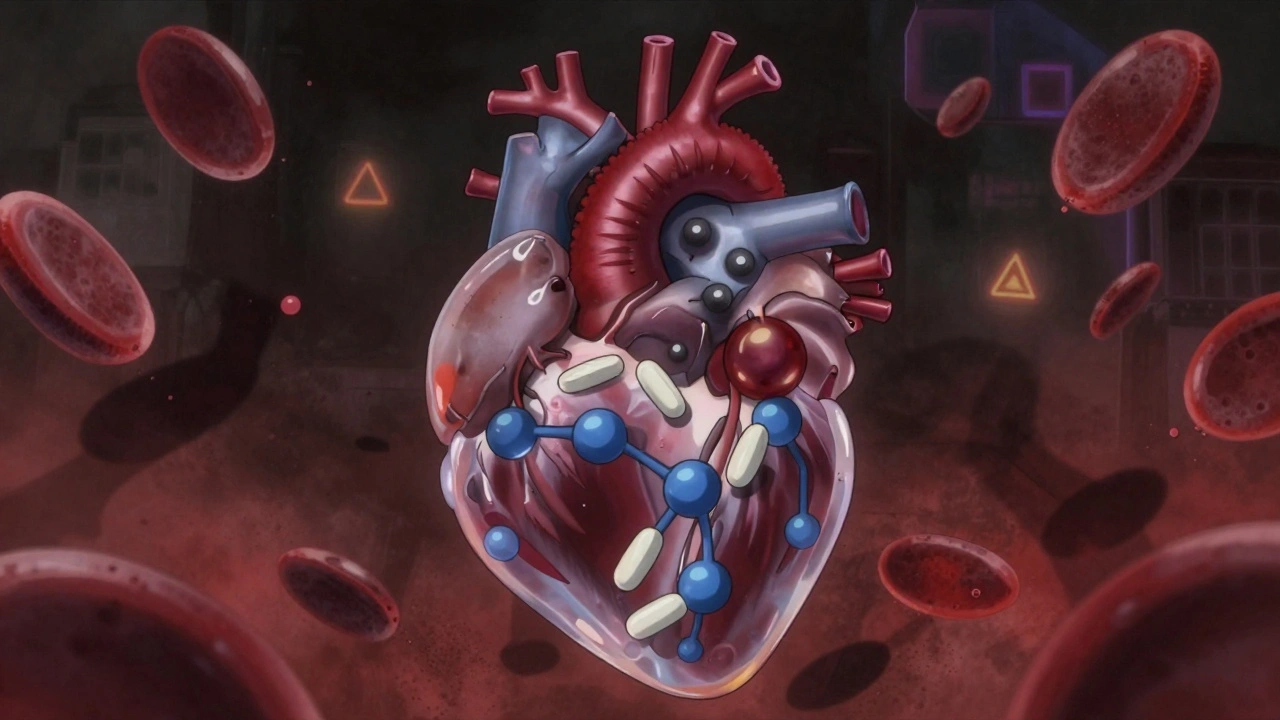
When your blood clots too easily, it can block arteries and trigger a heart attack or stroke. That’s where antiplatelet effects, the biological process that stops platelets from sticking together to form clots. Also known as antiplatelet therapy, it’s a key tool in preventing cardiovascular events. Unlike anticoagulants that target clotting factors, antiplatelet drugs work directly on platelets—the tiny blood cells that rush to injury sites and clump together. Think of them as traffic cops for your bloodstream, stopping platelets from forming dangerous roadblocks.
Drugs like aspirin, a common, low-cost antiplatelet agent that blocks the enzyme COX-1 to reduce platelet activation and clopidogrel, a prescription drug that stops ADP from signaling platelets to stick are used daily by millions. They’re often prescribed after stents, heart attacks, or for people with a history of stroke. But they’re not interchangeable. Aspirin works fast and cheap, while clopidogrel targets a different pathway—sometimes both are used together, especially after a stent placement. The goal isn’t to stop all clotting—just the kind that causes trouble.
Not everyone responds the same way. Some people have genetic variations that make clopidogrel less effective, a problem doctors now test for in high-risk cases. Others experience side effects like stomach irritation or unusual bruising. And while these drugs save lives, they aren’t risk-free. Taking them without medical reason can lead to dangerous bleeding. That’s why they’re not OTC for most people—your doctor needs to weigh the benefit against the risk.
What you’ll find below are real, practical guides on how these drugs work, how they compare to each other, what to watch for, and how they fit into broader treatment plans. You’ll see how bioequivalence testing ensures generics work the same as brand names, how drug interactions can turn a safe combo into a dangerous one, and why some people need double-checks before taking high-alert meds like these. These aren’t theory pieces—they’re based on real patient experiences, clinical data, and what actually happens in clinics and pharmacies.