Cholestyramine: What it is and how to use it
Cholestyramine is a bile acid sequestrant that helps lower LDL cholesterol and treats problems caused by excess bile acids in the gut. You usually get it as a powder to mix with water, milk, or fruit juice. Doctors prescribe it for high cholesterol when other drugs are not enough, for watery diarrhea caused by bile acid malabsorption, and for itching related to bile salts in liver disease.
How cholestyramine works and common uses
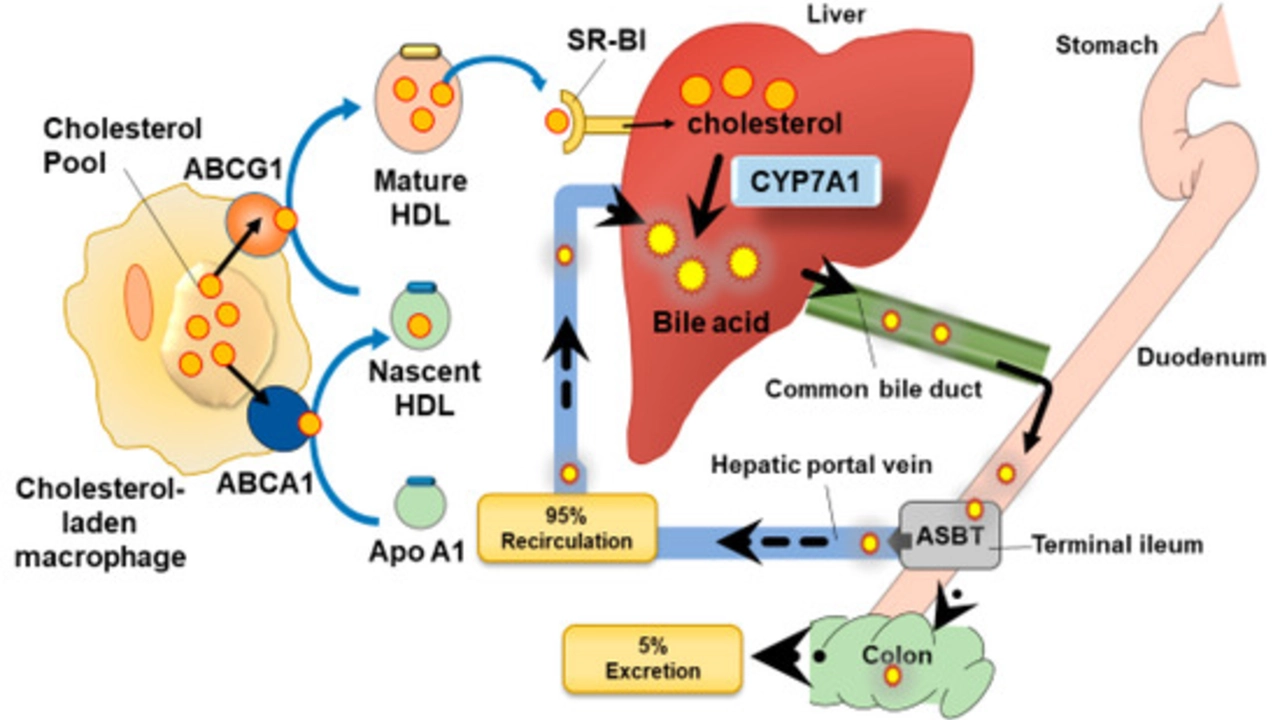
The medicine binds bile acids in the intestine so they cannot be reabsorbed. That lowers blood cholesterol because the liver then pulls more cholesterol from the blood to make new bile acids. For diarrhea, binding bile acids reduces their irritating effect on the colon. For itching from liver problems, cholestyramine reduces bile salts that build up and trigger itch.
Typical uses include: lowering LDL cholesterol, treating bile acid diarrhea after gallbladder removal or ileal disease, and easing cholestatic pruritus (bile salt itching). Your healthcare provider will explain the specific reason for your prescription and the expected benefits.
How to take it, side effects, and interactions
Follow your prescriber's dose. Powder usually mixes with 60–120 ml (2–4 oz) of fluid per dose. Stir until smooth and drink right away; add more fluid to rinse the cup. Take other oral medicines at least 1 hour before or 4–6 hours after cholestyramine to avoid reduced absorption. Examples of drugs affected include levothyroxine, warfarin, digoxin, and some fat-soluble vitamin supplements.
Common side effects are constipation, bloating, gas, and nausea. Increasing fiber and fluids helps with constipation. Less common but serious problems include severe constipation, bowel obstruction, and allergic reactions. Cholestyramine can reduce absorption of vitamins A, D, E, and K with long-term use, so your doctor may monitor levels or suggest supplements.
Store the powder at room temperature and keep the container tightly closed. If you miss a dose, take it when you remember unless it is close to the next dose. Do not double up without checking with your prescriber.
When to call your doctor: if you have severe belly pain, persistent vomiting, black or bloody stools, new or worsening jaundice, or signs of an allergic reaction like rash and trouble breathing. Mention pregnancy or breastfeeding plans—your provider will weigh risks and benefits.
If you want an alternative, ask about other bile acid sequestrants such as colesevelam or colestipol, or different cholesterol medicines like statins or ezetimibe. Your choice will depend on the reason for treatment, other health issues, and drug interactions.
Practical tips: start at the lowest prescribed dose and increase only if needed. Mix the powder with a full glass of fluid to avoid throat irritation and swallow any residue. Keep a list of all medicines and vitamins and show it to every provider. If you take blood thinners or thyroid medication, ask for blood tests after starting cholestyramine so doses can be adjusted. Report any sudden weight loss or worsening symptoms right away and keep follow up appointments.