CYP2C19: How Your Genes Affect Drug Response and Safety
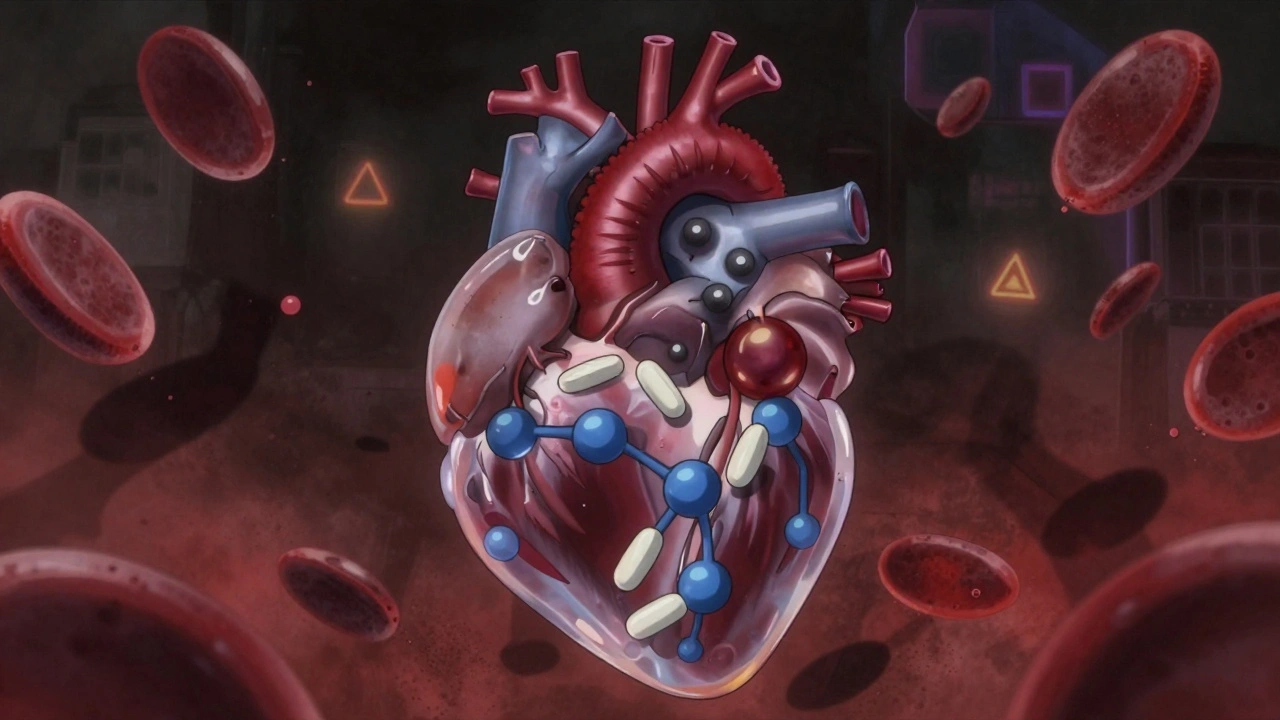
When your body breaks down medicine, it doesn’t treat all drugs the same. One of the main players in this process is CYP2C19, a liver enzyme encoded by the CYP2C19 gene that metabolizes nearly 10% of commonly prescribed drugs. Also known as cytochrome P450 2C19, it’s responsible for turning drugs like clopidogrel, proton pump inhibitors, and some antidepressants into forms your body can use—or eliminate. If your version of this gene works too slowly, too quickly, or not at all, your medication might not work, or worse, it could harm you.
People with certain CYP2C19 variations are called poor metabolizers, intermediate, extensive, or ultrarapid. A poor metabolizer might take a standard dose of clopidogrel—commonly prescribed after a heart attack—and still have a second one because the drug never activated properly. On the flip side, an ultrarapid metabolizer might clear anti-anxiety meds like diazepam so fast they get no relief. This isn’t guesswork. Studies show CYP2C19 status affects how well 30+ drugs work, including those used for depression, acid reflux, and blood clot prevention. It’s not just about side effects—it’s about whether the pill in your hand actually does what it’s supposed to.
That’s why pharmacogenomics, the study of how genes affect drug response is no longer science fiction. It’s showing up in hospital labs and prescribing guides. Doctors are starting to test for CYP2C19 before prescribing certain drugs, especially when the stakes are high—like after a stent placement or for someone with treatment-resistant depression. And it’s not just CYP2C19. This gene doesn’t work alone. It’s part of a network that includes CYP2D6, another major drug-metabolizing enzyme that affects pain meds, antipsychotics, and beta-blockers. When both genes are considered together, the picture of your drug response becomes much clearer.
What you’ll find in the posts below isn’t theory. It’s real-world guidance on how genetic differences like CYP2C19 impact everyday medication choices. You’ll see how people with slow metabolism get stuck with ineffective drugs, how generic switches can backfire if your genes aren’t taken into account, and why some patients suffer side effects even when they take their pills exactly right. These aren’t rare cases—they’re common, overlooked, and fixable. If you’ve ever wondered why a drug worked for your friend but not you, or why your doctor changed your meds after a blood test, this collection explains exactly why.