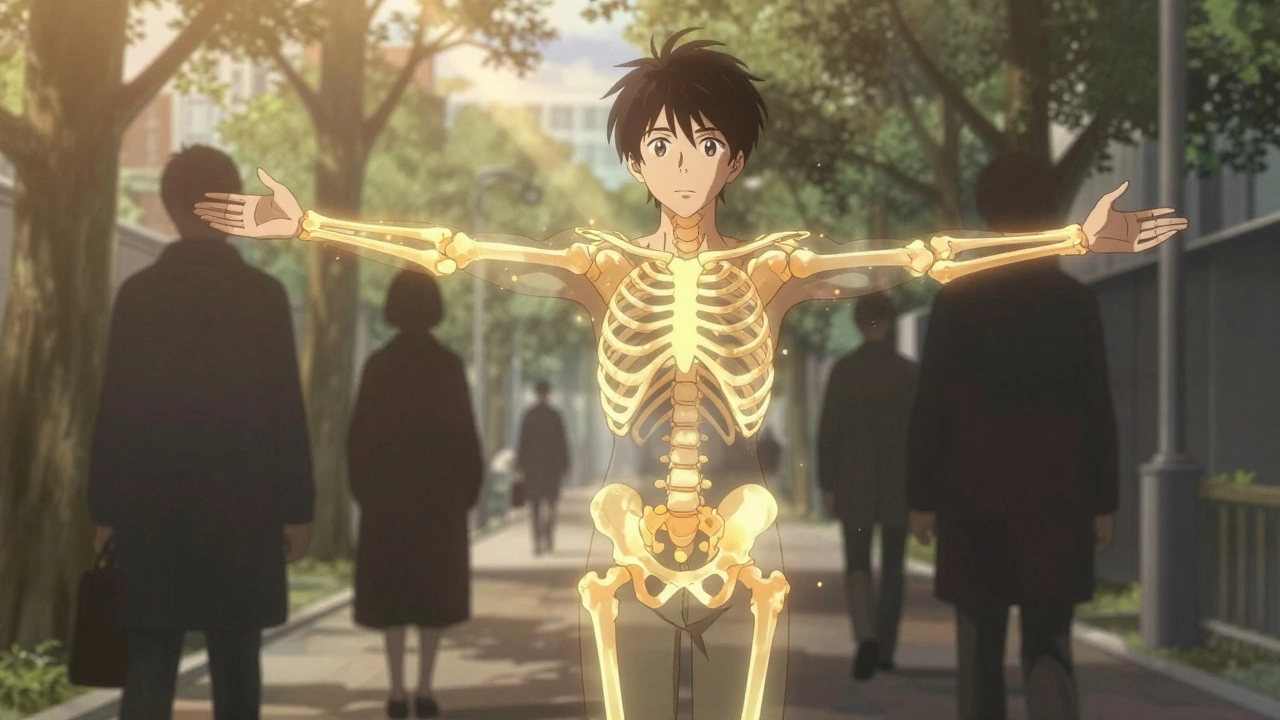
Why Vitamin D Matters for Your Bones
Every time you walk, climb stairs, or carry groceries, your bones are working hard. But without enough vitamin D, they can’t do their job properly. Vitamin D isn’t just a supplement you take because it’s trendy-it’s the key that unlocks your body’s ability to absorb calcium. Without it, your bones become porous, weak, and more likely to break. This isn’t theory-it’s science. In the early 1900s, doctors noticed children in industrial cities were developing soft, bent bones. They called it rickets. The cure? Sunlight and vitamin D. Today, we know vitamin D does more than prevent rickets. It keeps your bones dense, helps your muscles stay strong to prevent falls, and supports the constant renewal of bone tissue.
What’s the Right Level of Vitamin D?
For years, doctors said you needed at least 30 ng/mL of 25-hydroxyvitamin D in your blood to be healthy. That’s what the Endocrine Society recommended. But recent studies are flipping that idea on its head. The VITAL trial, led by Harvard researchers and tracking over 25,000 people for five years, found no difference in fracture rates between people taking 2,000 IU of vitamin D daily and those taking a placebo. Even more surprising? People with blood levels above 30 ng/mL didn’t have stronger bones than those with levels around 20 ng/mL. The Institute of Medicine still says 20 ng/mL is enough for 97% of people. That’s a big shift. If you’re healthy, active, and get some sun, you might already be getting what you need. Testing your vitamin D level isn’t always necessary unless you have risk factors like osteoporosis, dark skin, obesity, or limited sun exposure.
The Dangerous Myth of More Is Better
Many people think taking more vitamin D means stronger bones. That’s not true-and it can actually hurt you. A 2020 JAMA study gave people 400 IU, 4,000 IU, or 10,000 IU of vitamin D daily for three years. Those taking the highest doses ended up with lower bone density in their wrists and shins. The 10,000 IU group lost more bone than the 400 IU group. Why? Too much vitamin D can throw off calcium balance. Your body starts pulling calcium from your bones instead of putting it in. This isn’t speculation. It’s measured data from real bone scans. If you’re taking 5,000 IU or 10,000 IU daily without a doctor’s advice, you might be doing more harm than good. The sweet spot for most people? 600-800 IU. Higher doses should only be used if you’re deficient-and even then, only under medical supervision.
Supplements vs. Diet: What Actually Works?
Can you get enough vitamin D from food alone? Hardly. A 3-ounce serving of salmon has about 570 IU. A cup of fortified milk? 100 IU. One egg yolk? Just 44 IU. Even with a perfect diet, most people fall short. That’s why supplements are common. But not all supplements are created equal. ConsumerLab tested 20 brands in 2022 and found 15% contained less than 90% of the labeled dose. One brand had only 72% of what it claimed. On the flip side, another exceeded its label by 28%. If you’re going to take a supplement, choose one with third-party testing-look for USP, NSF, or ConsumerLab seals. Also, take it with your biggest meal. Vitamin D is fat-soluble. Taking it with dinner, especially if there’s some fat in the meal, boosts absorption by nearly 60% compared to taking it on an empty stomach.

Who Really Needs Extra Vitamin D?
Not everyone needs supplements. But some people do. If you’re over 65, have dark skin, live in a place with long winters (like the UK), wear full clothing for religious or cultural reasons, or have a BMI over 30, your body struggles to make or use vitamin D effectively. Obesity traps vitamin D in fat tissue, so people with higher BMI need nearly double the dose to reach the same blood levels. The Endocrine Society recommends 1,500-2,000 IU daily for obese adults. Postmenopausal women and older men with osteoporosis or a history of fractures should also consider supplementation, but only after testing their levels. For healthy people under 50 with regular sun exposure and a balanced diet, extra supplements likely offer no added benefit.
The Calcium Connection
Vitamin D doesn’t work alone. It needs calcium to build bone. But here’s the twist: taking calcium and vitamin D together doesn’t always help. A 2023 meta-analysis found that calcium-vitamin D combos reduced hip fracture risk by 30%-but only when vitamin D was under 400 IU per day. At higher doses, the benefit disappeared. Why? Too much vitamin D might cause calcium to deposit in the wrong places-like arteries instead of bones. Also, high-dose calcium supplements can cause constipation, kidney stones, or stomach upset. If you’re getting enough calcium from dairy, leafy greens, or fortified foods, you probably don’t need extra pills. The goal isn’t to max out both nutrients-it’s to balance them. Most adults need 1,000-1,200 mg of calcium daily. That’s about three servings of milk or yogurt, or a mix of tofu, almonds, and broccoli.
What About Sunlight?
Your skin makes vitamin D when exposed to sunlight. But in the UK, from October to March, the sun isn’t strong enough for your body to produce it. Even in summer, if you’re wearing sunscreen (which you should), you’re blocking most vitamin D synthesis. Still, 10-15 minutes of midday sun on your arms and face, two or three times a week, can help. No need to burn. Just enough to feel a little warmth. People with darker skin need longer exposure-up to three to six times as long-because melanin reduces vitamin D production. If you’re indoors all day, work night shifts, or live in a city with heavy pollution, you’re at higher risk for deficiency. But don’t rely on sun alone. Combine it with diet and, if needed, a low-dose supplement.

What’s Changing in the Medical World?
The tide is turning. Five years ago, doctors routinely prescribed 2,000 IU or more of vitamin D to older adults. Now, the American Geriatrics Society reports a 22% drop in those prescriptions since 2020. Why? Because the evidence didn’t hold up. The US Preventive Services Task Force says there’s no reason to take vitamin D supplements to prevent fractures in healthy adults. The International Osteoporosis Foundation still recommends supplementation for high-risk groups, but even they now emphasize testing first. New research is looking at personalized approaches-using genetics, BMI, and baseline levels to tailor doses. In Japan, a synthetic vitamin D analog called eldecalcitol is already used to treat osteoporosis with better results than standard supplements. That’s the future: not blanket recommendations, but smart, individualized care.
Practical Tips for Stronger Bones
- Get your vitamin D level checked if you’re over 50, have osteoporosis, or rarely get sunlight.
- If you’re deficient (below 20 ng/mL), start with 1,000-2,000 IU daily for 3 months, then retest.
- If you’re not deficient, stick to 600-800 IU daily-no more.
- Take your supplement with your largest meal, especially if it contains fat.
- Choose supplements with USP or NSF certification to avoid underdosed products.
- Get calcium from food first: yogurt, cheese, sardines, kale, fortified plant milks.
- Move your body: weight-bearing exercise like walking, dancing, or lifting weights strengthens bones more than any pill.
When to See a Doctor
Don’t self-prescribe high doses. If you have kidney disease, sarcoidosis, or a history of kidney stones, too much vitamin D can be dangerous. If you’re taking medications like steroids, anticonvulsants, or weight-loss drugs, they can interfere with vitamin D metabolism. Talk to your doctor before starting any new supplement-especially if you’re already on medication for bone health. A simple blood test can tell you if you’re truly deficient. And if you’ve had a fracture after a minor fall, your doctor might recommend a bone density scan (DXA) to check for osteoporosis.
Is it safe to take 5,000 IU of vitamin D daily?
For most healthy people, 5,000 IU daily is not recommended. Studies show no extra bone benefit at this dose-and it may lower bone density over time. Only take this amount if you’re severely deficient and under medical supervision. Long-term use above 4,000 IU can raise calcium levels dangerously, leading to kidney problems or heart issues.
Can you get enough vitamin D from food alone?
It’s very hard. Even eating fatty fish, eggs, and fortified milk every day won’t get most people to the recommended level. Sunlight helps, but in the UK, it’s not reliable from October to March. For most adults, a low-dose supplement (600-800 IU) is the easiest way to fill the gap without risking harm.
Do vitamin D supplements prevent fractures?
Only in people who are deficient. The VITAL trial and other large studies found no reduction in fractures for healthy adults taking daily supplements. But in those with low baseline levels, even 800 IU daily with calcium reduced hip fractures by nearly 30%. The key isn’t taking more-it’s fixing a true deficiency.
How long does it take for vitamin D to improve bone density?
It takes months. Vitamin D levels stabilize about 3 months after starting or changing a dose. Bone density changes take even longer-usually 12 to 24 months to show up on a DXA scan. Don’t expect quick results. Consistency matters more than high doses.
Should I take vitamin D3 or D2?
Vitamin D3 (cholecalciferol) is the better choice. It’s the form your skin makes from sunlight and is about 87% more effective at raising blood levels than D2 (ergocalciferol), which comes from plants. Most supplements now use D3. If you’re vegan, look for lichen-derived D3-it’s plant-based and just as effective.
Final Thought: Less Is Often More
For strong bones, you don’t need megadoses. You need balance. Enough vitamin D to absorb calcium. Enough calcium to build bone. Enough movement to keep bones stimulated. And no more than that. The hype around vitamin D has led many to over-supplement-and that’s where the real risk lies. If you’re healthy, active, and eat well, your bones are likely doing fine. If you’re unsure, get tested. Don’t guess. Your bones will thank you.

Jack Arscott
December 1, 2025 AT 14:03Lydia Zhang
December 1, 2025 AT 21:36Matt Dean
December 2, 2025 AT 17:09Adrian Barnes
December 4, 2025 AT 03:42Michelle Smyth
December 5, 2025 AT 21:01soorya Raju
December 6, 2025 AT 23:48Kay Lam
December 7, 2025 AT 06:09Walker Alvey
December 7, 2025 AT 06:33Patrick Smyth
December 8, 2025 AT 16:52Louise Girvan
December 10, 2025 AT 03:50Tommy Walton
December 12, 2025 AT 00:47James Steele
December 13, 2025 AT 05:50Dennis Jesuyon Balogun
December 13, 2025 AT 13:33Adrian Barnes
December 15, 2025 AT 00:00