When you pick up a prescription at the pharmacy, you might see two options: the brand-name drug you’ve heard of, or a cheaper generic version. You might wonder-does the generic really work the same? Is it just a copycat with cheaper ingredients? The answer lies in something called bioequivalence testing. This isn’t marketing. It’s science. And it’s the reason millions of people safely use generic drugs every day.
What Bioequivalence Testing Actually Measures
Bioequivalence testing doesn’t check if a drug cures the same disease. That’s already proven by the brand-name version. Instead, it answers one simple question: Does the generic drug get into your bloodstream at the same rate and in the same amount as the brand?
The FDA requires that generic drugs match the brand in three key ways: same active ingredient, same strength, same dosage form (pill, injection, etc.), and same route of administration (oral, topical, etc.). But that’s just the start. Two pills can look identical and still behave differently in your body. That’s where bioequivalence comes in.
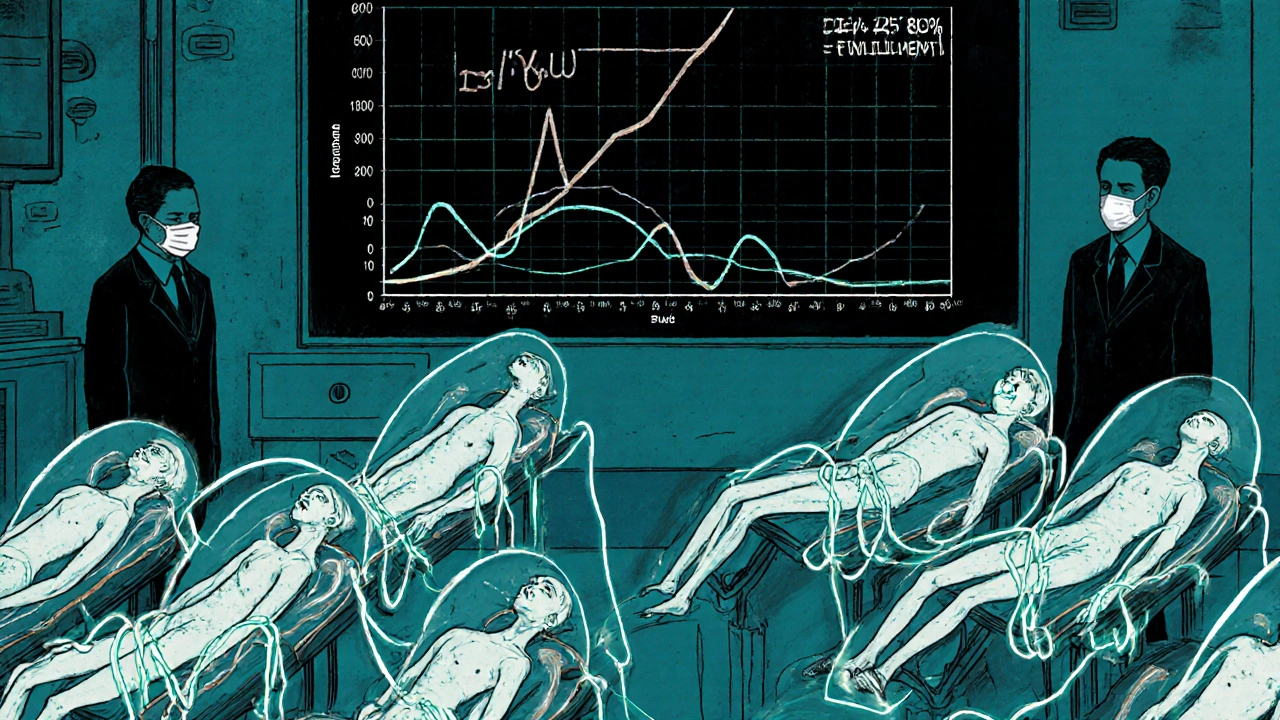
Researchers give 24 to 36 healthy volunteers both the brand and the generic version-sometimes one first, then the other, in a crossover design. Blood samples are taken over hours to track how much of the drug enters the bloodstream and how fast. Two numbers matter most: AUC (area under the curve), which measures total drug exposure over time, and Cmax, which shows the peak concentration.
The generic must show both AUC and Cmax within 80% to 125% of the brand’s values. That’s not a wide range. It means the generic can’t be too slow to absorb or too strong too fast. If it’s outside that range, it’s rejected. This standard isn’t arbitrary-it’s based on decades of clinical data showing that drugs within this range produce the same therapeutic effect.
Why This Matters More Than You Think
Imagine you’re taking a blood pressure pill. If the generic version hits your bloodstream too slowly, your pressure might spike. If it hits too fast, you could get dizzy or have side effects. Bioequivalence testing prevents both.
For most drugs, like antibiotics or statins, this 80%-125% window is more than enough. But for drugs with a narrow therapeutic index-like warfarin, lithium, or levothyroxine-the margin is tighter. In those cases, regulators demand even stricter testing. Some generics for these drugs go through additional studies, sometimes even clinical endpoint trials, to prove they’re safe.
It’s not just about pills. Inhalers, eye drops, and topical creams are trickier. You can’t easily measure drug levels in the lungs or skin. For those, the FDA uses other methods: measuring how the drug releases from the device, comparing how it behaves in lab tests, or even running small clinical studies that look at symptom improvement instead of blood levels.
The system isn’t perfect, but it’s built on real-world evidence. The FDA inspects over 1,200 generic drug factories every year. Manufacturers must follow strict quality rules-Good Manufacturing Practices-to ensure every batch is consistent. A pill made in India today must behave the same as one made six months ago.
How Generic Drugs Are Approved Without Repeating Clinical Trials
Brand-name drugs go through years of testing: Phase I (safety in healthy people), Phase II (effectiveness in small groups), Phase III (large-scale trials with patients). That costs billions.
Generic manufacturers don’t repeat that. Thanks to the Hatch-Waxman Act of 1984, they can rely on the brand’s existing safety and efficacy data. All they need to prove is bioequivalence. That cuts development time from 10-15 years to under two, and cost from $1 billion to maybe $2 million.
This is why generics make up 90% of U.S. prescriptions but only 23% of drug spending. In 2020 alone, they saved the U.S. healthcare system $313 billion. That’s not just a number-it means people can afford insulin, heart meds, and antidepressants they otherwise couldn’t.
The FDA’s Orange Book lists every approved generic and its therapeutic equivalence rating. If a generic is rated AB, it means the FDA has confirmed it’s bioequivalent and interchangeable with the brand. You can trust that label.
What Bioequivalence Testing Doesn’t Prove
Bioequivalence doesn’t guarantee identical side effects. That’s because generics can have different inactive ingredients-fillers, dyes, preservatives. These don’t affect how the drug works, but they can trigger allergies or stomach upset in sensitive people.
Some patients report feeling different on a generic. That’s often because of changes in the pill’s coating, size, or shape-not because the drug itself behaves differently. A 2022 Consumer Reports survey found that 87% of users saw no difference between generic and brand versions. Only 4% said the generic worked less effectively. In most of those cases, switching back to the brand didn’t help either. The issue was likely psychological or related to placebo effects.
There’s also a myth that generics “take longer to work.” That’s false. If the Cmax is within 80%-125%, the drug reaches peak levels at essentially the same time. A generic aspirin doesn’t sit in your stomach longer than the brand. It dissolves, absorbs, and starts working just as fast.
Global Standards and the Future of Testing
The U.S. isn’t alone. The European Medicines Agency, Health Canada, Japan’s PMDA, and others use nearly identical bioequivalence standards. The International Council for Harmonisation (ICH) ensures global alignment. A generic approved in Australia will meet the same criteria as one approved in the U.S. or Germany.
But the field is evolving. For complex drugs-like long-acting injectables or inhaled corticosteroids-traditional blood tests aren’t enough. The FDA and EMA are now exploring computer modeling. Physiologically Based Pharmacokinetic (PBPK) models simulate how a drug moves through the body based on its chemistry, anatomy, and physiology. These models could reduce the need for human trials in some cases.
In 2023, the FDA launched a new initiative to modernize bioequivalence standards for topical, inhaled, and ophthalmic products. They’re working with manufacturers to develop better lab tests and measurement tools. The goal? Keep the same high bar for safety, but make testing smarter and more efficient.

What You Should Know as a Patient
If your doctor prescribes a brand-name drug, you can ask for the generic. It’s almost always cheaper. Your pharmacist can’t switch it without your consent in most states, but they’ll tell you if a generic is available.
Don’t assume generics are inferior. They’re held to the same standards. The FDA doesn’t approve a generic unless it performs the same as the brand. If you notice a change after switching-like new side effects or feeling worse-talk to your doctor or pharmacist. It’s rarely the active ingredient. More likely, it’s a filler or coating you’re sensitive to.
And if you’re worried about quality, check the FDA’s website. You can look up any generic drug and see if it’s approved, who makes it, and whether it’s rated AB. No need to guess. The data is public.
Bottom Line: Bioequivalence Works
Bioequivalence testing isn’t a loophole. It’s a rigorous, science-backed system that lets safe, effective, affordable drugs reach millions. It’s why a month’s supply of generic lisinopril costs $4 instead of $150. It’s why people with diabetes, high blood pressure, or depression can stick to their treatment plans.
Yes, there are edge cases. Yes, complex drugs need more work. But for the vast majority of prescriptions, bioequivalence testing proves one thing beyond doubt: generic drugs work just as well as brand-name drugs. You’re not saving money by settling for less. You’re getting the same medicine, at a fraction of the cost.
Are generic drugs as effective as brand-name drugs?
Yes. Generic drugs must prove bioequivalence to the brand-name version by matching the rate and amount of drug absorbed into the bloodstream. The FDA requires that the 90% confidence interval for both AUC and Cmax falls between 80% and 125% of the brand’s values. This ensures the generic works the same way in the body. Over 90% of prescriptions in the U.S. are filled with generics, and studies show they perform identically in real-world use.
Why do some people say generics don’t work as well?
Most reports of differences come from changes in inactive ingredients-like dyes, fillers, or coatings-that can cause minor side effects (e.g., stomach upset or allergic reactions) in sensitive individuals. These don’t affect how the active drug works. A 2022 Consumer Reports survey found only 4% of users felt generics were less effective, and in many cases, switching back to the brand didn’t improve symptoms. Psychological factors and placebo effects also play a role. The active ingredient is identical; any perceived difference is rarely due to potency or absorption.
Do bioequivalence tests apply to all types of medications?
Not all. Standard bioequivalence testing using blood samples works well for oral pills and liquids. But for inhalers, eye drops, creams, or long-acting injections, measuring drug levels in the blood isn’t practical. For these, regulators use alternative methods: dissolution testing in labs, pharmacodynamic studies (measuring symptom changes), or clinical endpoint trials. The FDA has specific guidance for each type of complex product to ensure equivalence without relying on traditional pharmacokinetic data.
How long does it take for a generic drug to be approved?
The FDA’s average review time for a generic drug application (ANDA) is 10 to 12 months. Bioequivalence studies themselves typically take 6 to 8 months to complete, including recruiting volunteers, running tests, and analyzing data. Once submitted, the FDA reviews the manufacturing process, labeling, and bioequivalence data. Under the Generic Drug User Fee Amendments (GDUFA), 95% of applications met the FDA’s performance goal date in 2022, showing the system is efficient without sacrificing standards.
Can I trust generics made overseas?
Yes. The FDA inspects all manufacturing facilities-whether in the U.S., India, China, or elsewhere-using the same strict standards. About 1,200 facilities are inspected annually. Generic drugs made abroad must meet U.S. quality, purity, and potency requirements just like those made domestically. The FDA also monitors adverse events and can recall products if quality issues arise. Over 50% of generic drugs sold in the U.S. are manufactured overseas, and none are approved without passing the same bioequivalence and GMP checks.
What’s the difference between bioequivalence and therapeutic equivalence?
Bioequivalence means two drugs have the same rate and extent of absorption into the bloodstream. Therapeutic equivalence means they can be expected to have the same clinical effect and safety profile. All bioequivalent drugs are considered therapeutically equivalent by the FDA, unless there’s evidence otherwise. The FDA’s Orange Book assigns an AB rating to drugs that meet both criteria. Some drugs may be bioequivalent but not rated AB if they have known formulation issues or if switching causes problems in specific populations.


Sean Hwang
November 15, 2025 AT 16:36Been taking generic lisinopril for 3 years now. Same pill, same results. My BP’s steady and my wallet’s happy. No drama.
Barry Sanders
November 17, 2025 AT 06:4280-125%? That’s a massive gap. You’re basically saying ‘close enough’ and calling it science. Glad my insurance makes me take it.
Chris Ashley
November 18, 2025 AT 18:33bro i switched to generic omeprazole and my stomach felt like it was being stabbed by a rusty spoon. turned out it was the dye. not the drug. but still. weird.
kshitij pandey
November 19, 2025 AT 16:29As someone from India where we make a lot of these generics, I’m proud we help people worldwide afford life-saving meds. The science is solid. Trust the process. 🙏
Brittany C
November 21, 2025 AT 14:57It’s worth noting that the 90% CI for AUC and Cmax must fall within the 80–125% range per FDA guidance, which is derived from pharmacokinetic variability thresholds established in the 1980s. The statistical power is robust, but for narrow-therapeutic-index agents, post-marketing surveillance remains critical.
Sean Evans
November 22, 2025 AT 03:44LOL you people act like generics are magic. My cousin’s kid had a seizure after switching to a generic levothyroxine. FDA’s asleep at the wheel. 🤡
Anjan Patel
November 23, 2025 AT 16:07They let Chinese factories make our pills? And you’re okay with that? I bet half of them are using sawdust and wishful thinking. This system is a joke. People are dying because of this.
Scarlett Walker
November 24, 2025 AT 16:27My grandma’s on 7 meds, 6 are generic. She says she feels better now because she actually takes them. That’s the real win. 💛