When you’re prescribed carbamazepine for seizures or nerve pain, you might assume all generics are the same. But if you’ve ever had a seizure return after a pharmacy switch, or felt dizzy and confused after a refill change, you’re not alone. Carbamazepine isn’t like taking a generic ibuprofen. Its enzyme induction and drug interactions make it one of the most dangerous drugs to swap between generic brands - even if they’re labeled "bioequivalent."
Why Carbamazepine Is Different
Carbamazepine was first approved in 1974 under the brand name Tegretol. Today, over 30 generic versions are on the market in the U.S. alone. On paper, they all meet FDA standards: they deliver the same amount of drug into the bloodstream within an 80-125% range compared to the brand. Sounds fair, right? But here’s the catch: carbamazepine has a narrow therapeutic index. That means the difference between a dose that works and one that causes harm is small. The therapeutic range is 4-12 mcg/mL. Go below 4, and seizures return. Go above 12, and you risk dizziness, nausea, blurred vision, or even life-threatening toxicity. Worse, carbamazepine doesn’t just sit in your body. It actively changes how your body processes other drugs - and even itself.Enzyme Induction: Your Liver Gets Overworked
Carbamazepine is a powerful inducer of CYP3A4, one of the main liver enzymes that break down drugs. Within 48 hours of starting it, your liver starts making more of this enzyme. By two to three weeks, it’s working at full speed. That means:- Carbamazepine speeds up its own breakdown - this is called autoinduction. Your body gets used to it fast, which is why doses often need to be increased over time.
- It reduces levels of other drugs you’re taking. Warfarin? Less effective. Birth control pills? Might not work. Cyclosporine? Risk of organ rejection. HIV meds? Could fail.
- It also boosts UGT enzymes and P-glycoprotein, which push drugs out of your cells. That affects even more medications - from antidepressants to chemotherapy.
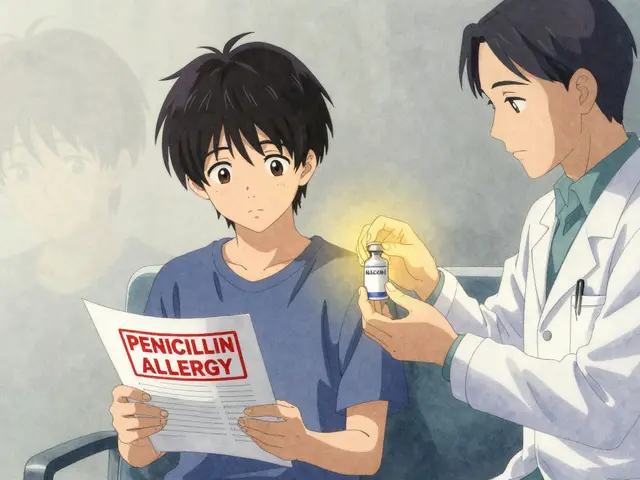
Generic Switches Can Trigger Seizures - Even When They’re "Bioequivalent"
Here’s where things get real. A 2018 study in Epilepsia followed 327 patients who were switched between different generic carbamazepine brands. Twelve percent had breakthrough seizures or severe side effects. Nearly 8% ended up in the ER. Why? Because bioequivalence studies are done in healthy young volunteers. Not in people with epilepsy, liver disease, or who are taking five other meds. The European Medicines Agency classifies carbamazepine as a narrow therapeutic index (NTI) drug. The FDA agrees. That’s why they tightened testing for extended-release versions in 2023 - requiring stricter dissolution profiles across different pH levels in the gut. But here’s the problem: one generic might use a different coating or bead size than another. A patient with gastroparesis (delayed stomach emptying) might absorb one version perfectly but struggle with another. A Reddit user named NeuroNurse2020 pointed out that Nostrum’s extended-release capsules have different bead sizes than others - and that matters for people with digestive issues. One patient, "SeizureFree87," posted on the Epilepsy Foundation forum: "I switched from Tegretol XR to a generic. My carbamazepine level dropped from 7.2 to 4.8 mcg/mL. Seizures went from once a month to four or five a week. Same dose. Same doctor. Just a different pill."
Gender, Genetics, and Metabolism
Men and women process carbamazepine differently. Women have higher CYP3A4 activity - meaning they break it down faster. That’s why a 2021 study in Pharmacogenetics and Genomics found women need slightly higher doses on average. And it gets more complex. A 2021 JAMA Neurology study showed women of childbearing age had 22% more breakthrough seizures after switching generics. Why? Hormones. Estrogen boosts CYP3A4. So during ovulation or when on birth control, carbamazepine levels can dip - even if you haven’t switched brands. Genetics matter too. About 17 genetic variations affect how fast carbamazepine is metabolized. People with the CYP3A4*22 variant need 25% less drug to reach safe levels. Without testing, they’re at risk of toxicity.The HLA-B*1502 Warning - A Life-or-Death Genetic Risk
If you’re of Asian descent - Chinese, Thai, Malaysian, Filipino, or other Southeast Asian ancestry - you must be tested for the HLA-B*1502 gene before starting carbamazepine. This isn’t a "maybe." The FDA issued a black box warning in 2007. People with this gene have a 10-fold higher risk of Stevens-Johnson Syndrome (SJS) - a deadly skin reaction that can kill. Incidence? 5.9 cases per 1,000 in HLA-B*1502-positive patients. 0.6 per 1,000 in those without it. That’s not a small risk. It’s a dealbreaker. For these patients, levetiracetam or lamotrigine are safer first choices. Carbamazepine should only be used if no alternatives exist - and only after genetic testing.
What You Should Do - Practical Steps
If you’re on carbamazepine, here’s what actually works:- Never switch generics without telling your doctor. Even if your pharmacy says "it’s the same."
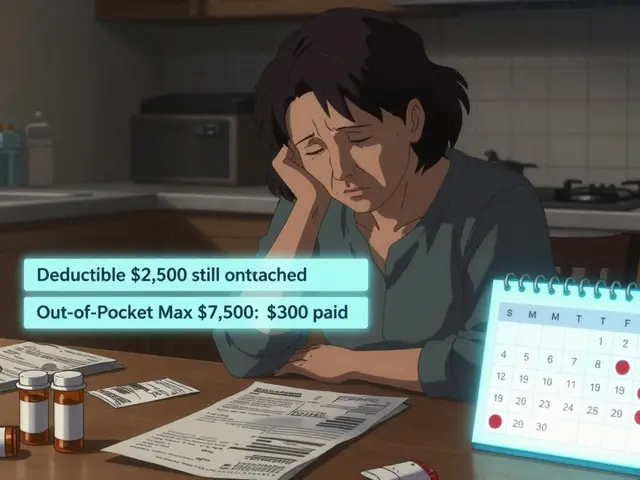
- Ask for "dispense as written" (DAW 1) on your prescription. This stops automatic substitution. 68% of U.S. neurologists already do this for carbamazepine patients.
- Get a blood test before and after any switch. Check levels at baseline, then again at 7-10 days and 4 weeks after switching. If levels drop or rise by more than 15%, your dose needs adjusting.
- Know your manufacturer. The FDA’s Orange Book lists 12 different makers of 200 mg carbamazepine tablets. Write down the name on your pill bottle. If it changes, call your doctor.
- Ask about genetic testing. If you’re of Asian descent, get HLA-B*1502 tested. If you’ve had unexplained rashes or liver issues on carbamazepine, consider pharmacogenetic screening.


Uzoamaka Nwankpa
January 4, 2026 AT 13:41My cousin went from Tegretol to a generic and started having seizures every other day. The pharmacy said it was the same. Same dose. Same doctor. But her blood levels dropped like a rock. They didn’t even test her until she ended up in the ER. This isn’t just about pills-it’s about your life.
Chris Cantey
January 5, 2026 AT 23:39It’s not just carbamazepine. It’s the entire pharmaceutical industrial complex pretending bioequivalence is a scientific absolute when it’s really a statistical approximation designed to maximize profit margins. We’ve outsourced our biology to corporate compliance forms.
Abhishek Mondal
January 7, 2026 AT 15:12Let’s be precise: the FDA’s 80–125% bioequivalence window is mathematically indefensible for NTI drugs-especially when CYP3A4 autoinduction introduces nonlinear pharmacokinetics. The dissolution profile variance between bead formulations is not merely ‘a difference’-it’s a pharmacodynamic catastrophe waiting to happen. And yes, I’ve read the 2023 FDA guidance on extended-release carbamazepine dissolution under pH 1.2–6.8 conditions. The data is alarming.
Oluwapelumi Yakubu
January 8, 2026 AT 00:38Man, this is wild. I used to work in a pharmacy in Lagos, and we had a guy on carbamazepine who kept having seizures after switching generics. We didn’t even have blood testing there, but we learned quick: if the pill looked different, we warned him. One brand had these little blue beads, another had white ones. He said the white ones made him feel like his brain was underwater. Turns out, the coating was different. No fancy lab needed-just a patient who paid attention.
Terri Gladden
January 9, 2026 AT 13:47So like... my sister switched to a generic and started getting rashes? Like, full-on peeling skin? And the doctor was like "oh maybe it's allergies"? NO. It was the damn pill. And now she's terrified to take ANYTHING. Like, what even is medicine anymore? I just want to take a pill and not die.
Jennifer Glass
January 11, 2026 AT 02:09I appreciate how thorough this is. I’m a nurse and we’ve had several patients come in with unexplained drops in carbamazepine levels after a pharmacy switch. We always check the manufacturer name now-write it down, take a picture. It’s a small thing, but it saves lives. Also, the HLA-B*1502 testing point is critical. I’ve seen people from Southeast Asia prescribed this without a single question. That’s negligence.
Joseph Snow
January 12, 2026 AT 18:45This is all part of the government’s plan to make people dependent on expensive brand-name drugs. The FDA is in bed with Big Pharma. Why else would they allow generics at all if they’re so dangerous? They want you to keep buying Tegretol. They’re scared of competition. The real issue isn’t the pill-it’s the system that lets them profit off your fear.
John Ross
January 13, 2026 AT 01:15Let’s not mince words: carbamazepine is a pharmacokinetic nightmare. The CYP3A4 induction cascade, coupled with P-gp upregulation and UGT modulation, creates a dynamic, non-linear metabolic landscape that renders static bioequivalence models obsolete. The 2022 J Clin Pharm Ther study’s 65–75% TDM requirement isn’t a recommendation-it’s a baseline survival protocol. Any prescriber who doesn’t mandate serial levels is practicing malpractice by omission.
Clint Moser
January 13, 2026 AT 22:07Did you know the FDA doesn’t test generics in people with epilepsy? They test them in college kids who’ve never had a seizure. That’s why they’re lying to us. And the bead sizes? They’re changing them on purpose. The government wants you to have seizures so you’ll go back to the brand-and they get kickbacks from the pharma companies. I’ve got the documents. It’s all connected.
Ashley Viñas
January 14, 2026 AT 06:25I’m sorry, but if you can’t afford Tegretol, maybe you shouldn’t be on a drug that requires blood tests every month. This isn’t aspirin. It’s a high-maintenance, high-risk medication. If you’re going to take it, you need the resources to manage it. Otherwise, you’re just putting your life-and your family’s peace of mind-at risk. It’s not fair to the system.
Brendan F. Cochran
January 15, 2026 AT 09:31Why are we letting foreign labs make our meds? India and China are pumping out these generics like candy. And now people are having seizures because some guy in Bangalore used the wrong dye? This is why America needs to bring pharma back home. No more outsourcing our safety. Tegretol is American. The generics? Foreign garbage.
jigisha Patel
January 16, 2026 AT 21:36While the article correctly identifies NTI risks, it fails to contextualize the cost-benefit calculus in low-resource settings. In Nigeria and rural India, Tegretol is unaffordable. The 12% seizure recurrence rate in the Epilepsia study must be weighed against the 98% non-adherence rate if generics are withheld. The solution isn’t prohibition-it’s investment in TDM infrastructure. Blaming generics is convenient; fixing systems is hard.
Mandy Kowitz
January 18, 2026 AT 03:21Wow. So the whole thing is just a scam. And we’re supposed to believe the FDA? LOL. My cousin took the generic, got dizzy, and the pharmacist said "it’s just your body adjusting." Like, no. It’s the pill. They know. They just don’t care.