When your potassium levels climb too high, your heart doesn’t just skip a beat-it can stop. This isn’t a scare tactic. It’s what happens in hyperkalemia, a silent but deadly condition triggered by common medications millions take every day. Many people don’t realize their blood pressure pills, heart failure drugs, or even over-the-counter salt substitutes could be quietly pushing their potassium into the danger zone. And when that happens, the risk of sudden cardiac arrest rises fast.
What Is Hyperkalemia, and Why Does It Matter?
Hyperkalemia means your blood has too much potassium-above 5.5 mEq/L. Normal levels are between 3.5 and 5.0. At 6.5 or higher, you’re in severe territory. The problem isn’t just the number. It’s what that number does to your heart.
Potassium helps your heart muscle contract and relax. But when levels spike, the electrical signals that keep your heartbeat steady go haywire. You might not feel anything at first. No chest pain. No shortness of breath. Just a quiet, creeping danger. By the time symptoms like palpitations, muscle weakness, or nausea show up, it’s often too late. That’s why this condition catches so many off guard.
It’s not rare. About 2-3% of the general population has it. But if you’re on meds for high blood pressure, heart failure, or kidney disease, your risk jumps to 10-20%. And if you’re hospitalized? That number climbs even higher.
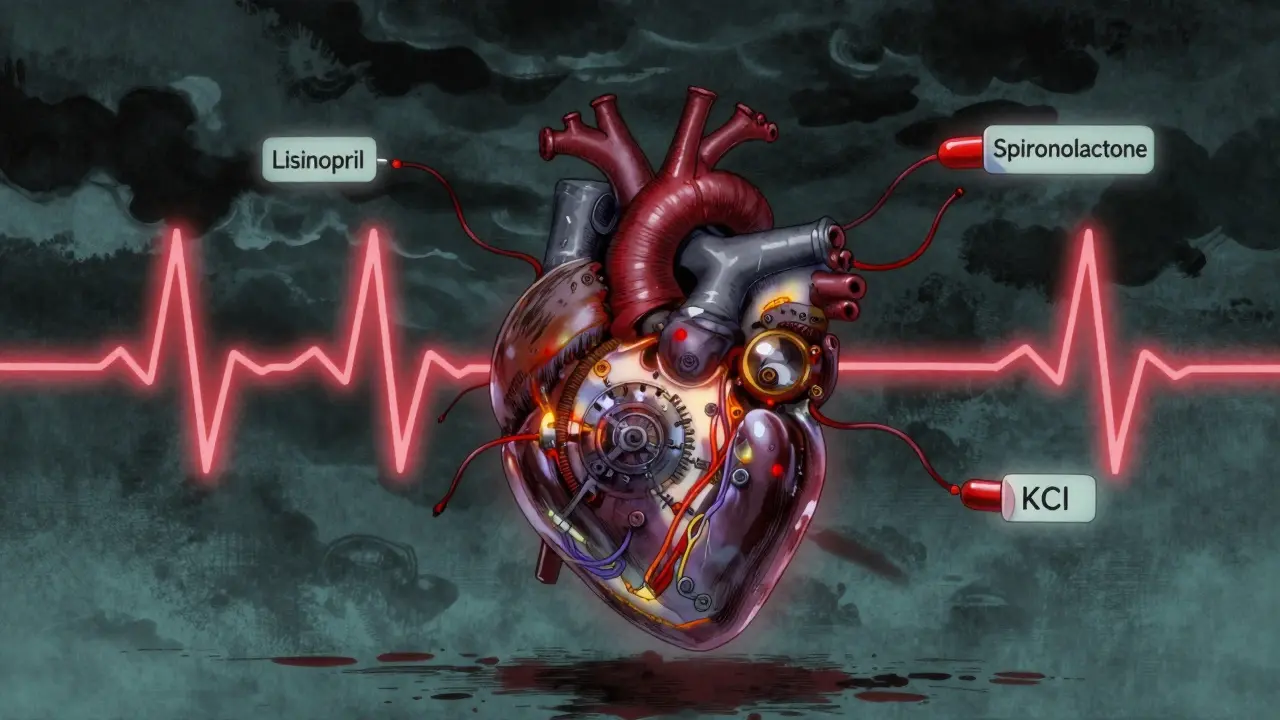
Which Medications Cause Hyperkalemia?
The biggest culprits are drugs that protect your heart and kidneys-but accidentally trap potassium in your blood. These include:
- ACE inhibitors like lisinopril
- ARBs like losartan
- Mineralocorticoid receptor antagonists like spironolactone
- Potassium-sparing diuretics like amiloride
- Direct renin inhibitors like aliskiren
These drugs are lifesavers. They lower blood pressure, reduce heart strain, and slow kidney damage. But they all interfere with how your body gets rid of potassium. And when you combine them-say, spironolactone with an ACE inhibitor-the risk multiplies. One study found that pairing those two with the antibiotic co-trimoxazole increased the risk of sudden death by more than five times.
Other factors make it worse: kidney disease (especially with eGFR under 60), diabetes, being over 65, or being dehydrated. Even skipping a dose of your diuretic can tip the scale.
The Cardiac Risks: What Happens Inside Your Heart
Your heart’s rhythm depends on a tight balance of electrical charges. Potassium plays a central role. When levels rise above 5.5 mEq/L, the resting membrane potential of heart cells starts to shift. That makes them more excitable-and more likely to fire randomly.
On an ECG, you’ll see the warning signs:
- Peaked T-waves at 5.5-6.5 mEq/L
- PR interval prolongation at 6.5-7.5 mEq/L
- QRS complex widening above 7.5 mEq/L
- Sine wave pattern just before ventricular fibrillation
At 6.5 mEq/L or higher, the risk of life-threatening arrhythmias spikes. The heart can’t pump properly. It might flutter, quiver, or stop entirely. Studies show patients with hyperkalemia are far more likely to suffer cardiac arrest, heart failure, or stroke in the hospital than those with normal potassium levels-even when they’re on the same heart meds.
And here’s the cruel twist: you might not feel a thing until it’s too late. That’s why regular blood tests are non-negotiable if you’re on these drugs.
How Is It Treated? Immediate Actions for Life-Threatening Cases
If your potassium hits 6.5 mEq/L or higher-or you have ECG changes-time is measured in minutes, not hours.
The first step? Calcium gluconate. Given intravenously, it doesn’t lower potassium. But it stabilizes the heart muscle, blocking the dangerous electrical changes. Effects kick in within 2-3 minutes and last about 30-60 minutes. It’s not a cure-it’s a shield.
Next, you shift potassium back into cells:
- Insulin and glucose: 10 units of insulin with 25 grams of glucose. Lowers potassium by 0.5-1.5 mEq/L in 15-30 minutes.
- Albuterol nebulizer: 50-100 mcg. Drops potassium by 0.5-1.0 mEq/L.
These are temporary fixes. They buy time. But you still need to get the excess potassium out of your body.
Long-Term Management: Keeping Your Heart Safe Without Stopping Your Meds
For years, the only answer to high potassium was to stop the meds that caused it. But that’s like turning off your heart pump because the battery’s low. You lose the protection you need.
Now, there’s a better way: potassium binders.
Two FDA-approved drugs-patiromer (Veltassa) and sodium zirconium cyclosilicate (Lokelma)-work in your gut. They trap potassium like a sponge and flush it out in your stool. Within hours, they lower potassium by 0.4-1.0 mEq/L.
Studies show that with these binders, 86% of patients stay on their heart-protective meds. Without them, 38% of people on high-dose RAASi drugs had to stop them because of mild hyperkalemia. That’s a huge win.
Side effects? Some people get constipation (15-20%) or diarrhea (10-15%). But for most, the trade-off is worth it.
What You Can Do at Home
Medications aren’t the only source of potassium. Your diet matters too.
If you’re at risk, aim for 2,000-3,000 mg of potassium daily. That means cutting back on:
- Bananas, oranges, potatoes, tomatoes
- Salt substitutes (they’re often pure potassium chloride)
- Processed foods with potassium additives
Stay hydrated. Dehydration concentrates potassium in your blood. Drink water unless your doctor says otherwise.
Check your labs regularly. If you’re on RAASi meds, get your potassium tested every 1-4 weeks, especially after a dose change or new medication.
And never stop your meds on your own. Talk to your doctor first. There are ways to keep you safe without giving up your heart protection.
The Bigger Picture: Why This Matters for Your Future Health
Hyperkalemia used to be seen as a reason to stop life-saving drugs. Now, it’s a treatable side effect. That’s a major shift in medicine.
With potassium binders, patients with heart failure and kidney disease can stay on their meds longer. That means fewer hospitalizations, fewer heart attacks, and longer lives. Modeling studies suggest this could improve cardiovascular outcomes by 20-25% in high-risk groups.
Doctors are learning to see hyperkalemia not as a failure of treatment-but as a signal to adjust it. The goal isn’t to avoid high potassium at all costs. It’s to manage it so you can keep getting the benefits of your heart and kidney meds.
If you’re on one of these drugs, ask your doctor: "Could my potassium be high? When was my last test? Do I need a binder?" Don’t wait for symptoms. The most dangerous cases have none.
Can hyperkalemia happen without symptoms?
Yes. Many people with mild to moderate hyperkalemia feel nothing at all. Symptoms like muscle weakness, nausea, or irregular heartbeat often appear only when potassium is dangerously high. That’s why regular blood tests are critical if you’re on medications like ACE inhibitors, ARBs, or spironolactone. Relying on symptoms alone can be deadly.
Is hyperkalemia always caused by medication?
No. While medications are the most common cause, other factors can raise potassium levels. These include kidney disease (especially advanced stages), uncontrolled diabetes, severe tissue injury (like burns or trauma), and rare hormonal disorders. But in the U.S. today, over 80% of hospital cases are linked to drugs-especially those used for heart and kidney conditions.
Can I take potassium supplements if I have high potassium?
Absolutely not. Potassium supplements, including salt substitutes labeled "lite" or "no sodium," can push your levels into the danger zone. Even some multivitamins or herbal products contain potassium. Always check labels and talk to your doctor before taking anything new. If you’re on a potassium binder, your doctor may still advise avoiding these entirely.
How long do potassium binders take to work?
Potassium binders like Lokelma and Veltassa start working within hours. Most people see a drop in potassium levels within 24-48 hours. They’re not for emergencies-they’re for long-term control. You’ll need to take them daily, usually with food, to keep potassium stable over time. They’re not a one-time fix, but they allow you to stay on your heart-protective medications safely.
What happens if I stop my blood pressure pill because of high potassium?
Stopping your RAAS inhibitor (like lisinopril or losartan) might lower your potassium-but it also removes vital protection for your heart and kidneys. Studies show patients who stop these drugs due to hyperkalemia have higher rates of heart failure hospitalizations and death. The modern approach is to use potassium binders to keep you on the meds that save your life, not to stop them. Always discuss alternatives with your doctor before making changes.


michelle Brownsea
January 21, 2026 AT 05:07Let me be perfectly clear: if you're taking ACE inhibitors or spironolactone and not monitoring your potassium, you're not managing your health-you're playing Russian roulette with your heart. This isn't hypothetical. I've seen it. A neighbor-62, diabetic, on lisinopril-collapsed at church. No warning. No symptoms. Just... gone. And the autopsy? Hyperkalemia. The doctor said, "It was preventable." So why do people still ignore labs? Because they trust pills more than science? Sad.
Malvina Tomja
January 21, 2026 AT 11:59Let’s be honest-this post is technically accurate but emotionally manipulative. You’re scaring people into compliance by invoking cardiac arrest without contextualizing risk magnitude. The absolute risk of sudden death from hyperkalemia in outpatient RAASi users is less than 0.3% annually. Meanwhile, the mortality reduction from these drugs is 20–30%. You’re conflating statistical hazard with imminent doom. That’s not medicine-it’s fearmongering dressed as education.
Samuel Mendoza
January 22, 2026 AT 00:12shubham rathee
January 23, 2026 AT 00:34MAHENDRA MEGHWAL
January 23, 2026 AT 13:48Thank you for this meticulously researched and clinically grounded exposition. The integration of pathophysiology, pharmacokinetics, and therapeutic strategy is exemplary. In particular, the delineation of ECG changes in relation to serum potassium thresholds demonstrates a profound understanding of cardiac electrophysiology. I would only add that serial monitoring should be institutionalized in primary care protocols for patients on RAAS inhibitors, particularly in comorbid populations. This is not merely clinical advice-it is public health imperative.
Kevin Narvaes
January 24, 2026 AT 07:19Kelly McRainey Moore
January 24, 2026 AT 19:20Amber Lane
January 25, 2026 AT 08:22Ashok Sakra
January 27, 2026 AT 02:02Andrew Rinaldi
January 28, 2026 AT 15:53I appreciate the depth of this post. It’s rare to see both the science and the human impact addressed with such balance. I’ve seen patients stop their meds out of fear, then end up in heart failure. I’ve also seen others ignore labs until it’s too late. The middle path-monitoring with binders-isn’t flashy, but it’s the most compassionate solution. Let’s normalize regular labs as part of routine care, not an afterthought.
Gerard Jordan
January 30, 2026 AT 05:59Roisin Kelly
January 31, 2026 AT 17:17lokesh prasanth
February 2, 2026 AT 15:41