Diabetic ketoacidosis, or DKA, isn’t just a scary term you hear in doctor’s offices-it’s a medical emergency that can kill someone within hours if ignored. It happens when your body doesn’t have enough insulin to use sugar for energy, so it starts burning fat instead. That process floods your blood with acidic ketones, throwing your whole system out of balance. And it doesn’t just affect people who’ve had diabetes for years. About 30% of kids diagnosed with type 1 diabetes show up in the ER with DKA because no one recognized the early signs. This isn’t rare. In the U.S. alone, over half a million hospital days each year are tied to DKA. The good news? If you know what to look for and act fast, you can stop it before it becomes life-threatening.
What Are the Early Warning Signs?
The first signs of DKA are easy to miss because they look like a bad flu or a stomach bug. You feel thirsty all the time-not just a little, but so much you’re drinking four to six liters of water a day. You’re peeing constantly, sometimes more than three liters in 24 hours. Your mouth feels like cotton. Your blood sugar is over 250 mg/dL, but you might not even check it because you feel fine otherwise. This stage usually starts within 4 to 12 hours and can last a full day before things get worse.Here’s what’s happening behind the scenes: without insulin, your cells starve for fuel. Your liver starts breaking down fat into ketones to compensate. These ketones are acids. As they build up, your blood becomes too acidic. That’s when you start feeling sick. Nausea hits around 75% of the time. Vomiting follows in 65%. Abdominal pain is common too-so much so that people often think they have appendicitis or food poisoning. Fatigue isn’t just being tired. It’s being so weak you can’t stand up or walk to the bathroom. Grip strength drops by 30 to 40% in clinical trials. You’re not lazy-you’re in metabolic crisis.
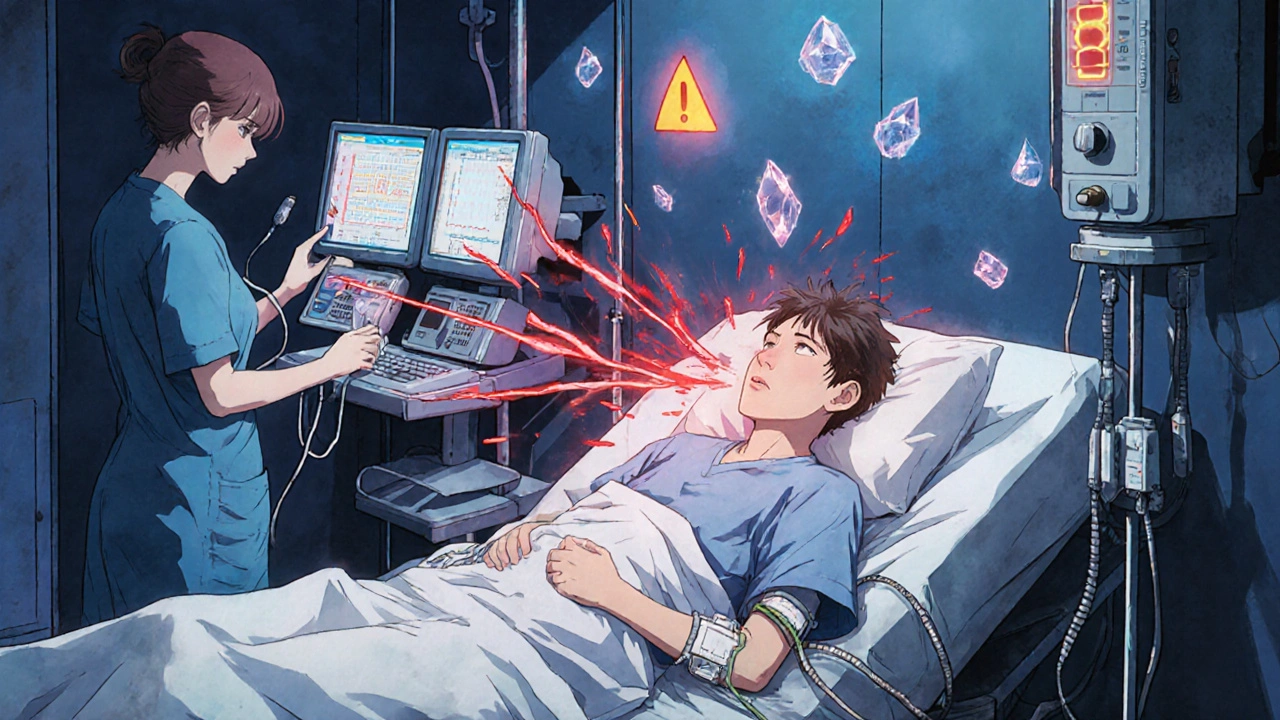
When It Gets Critical: Red Flags You Can’t Ignore
If you’ve had these symptoms for more than 12 hours and they’re getting worse, you’re entering danger territory. Your breathing changes. It becomes deep, fast, and labored-called Kussmaul breathing. This is your body’s last-ditch effort to blow off acid through your lungs. You might notice a fruity or nail polish remover smell on your breath. That’s acetone, the main ketone your body produces. It’s unmistakable once you’ve smelled it.Confusion sets in when your blood pH drops below 7.1. Disorientation, slurred speech, dizziness-these aren’t signs of being drunk or stressed. They’re signs your brain is being affected by acid. In 15% of severe cases, people lose consciousness before they even make it to the hospital. Children are especially vulnerable. Cerebral edema, or brain swelling, is the leading cause of death in kids with DKA, and it can happen even during treatment if fluids are given too fast. That’s why hospitals follow strict protocols.
How Hospitals Treat DKA: The Standard Protocol
There’s no debate about what to do once someone is diagnosed with DKA: get them to the hospital immediately. No home remedies. No waiting to see if it gets better. The treatment is standardized, evidence-based, and time-sensitive.First, fluids. You get 15 to 20 milliliters per kilogram of body weight of saline solution in the first hour-that’s about 1 to 1.5 liters for most adults. This isn’t just to rehydrate you. It flushes out ketones, restores blood volume, and helps your kidneys start working again. After that, fluids slow down to 250 to 500 mL per hour to avoid swelling the brain.
Next, insulin. You get a small IV bolus, then a continuous drip. The goal isn’t to drop your blood sugar fast. It’s to lower it slowly-50 to 75 mg/dL per hour. Too quick, and you risk cerebral edema, especially in children. The insulin drip continues until your ketones are gone, your blood pH is back above 7.3, and your bicarbonate is over 18 mmol/L. That usually takes 12 to 24 hours.
Electrolytes are just as important. Even if your blood test shows normal potassium, you’re actually severely depleted. Insulin pushes potassium into cells, which can crash your levels dangerously low. So doctors start replacing potassium as soon as your levels are below 5.2 mmol/L. Most patients need 20 to 30 mEq per hour. Sodium, chloride, and magnesium are also monitored closely.
Bicarbonate? Rarely used. Only if your pH is below 6.9-which is extremely rare. Giving bicarbonate can actually make things worse by increasing the risk of brain swelling. The American Diabetes Association says it’s unnecessary in 95% of cases.
What Triggers DKA-and How to Prevent It
DKA doesn’t come out of nowhere. It’s almost always triggered by something. In half of all cases, it’s an infection-pneumonia, urinary tract infection, even a bad cold. In 30% of cases, it’s because someone skipped insulin, either on purpose or by accident. And in 20% of cases, DKA is the first sign someone has type 1 diabetes.Insulin pump users are at higher risk during illness. If your infusion set gets clogged or dislodged, you stop getting insulin-even if the pump says it’s working. Tandem Diabetes Care recommends switching to injections when you’re sick. Don’t rely on the pump.
There’s also a newer form called euglycemic DKA. Your blood sugar might be under 250 mg/dL, but your ketones are still high. This happens mostly in people taking SGLT2 inhibitors (like Jardiance or Farxiga), even if they have type 1 diabetes. It’s easy to miss because the sugar isn’t sky-high. If you’re on one of these drugs and feel unwell, check your ketones-even if your glucose looks normal.
Technology Is Changing the Game
Continuous glucose monitors (CGMs) like Dexcom G7 have cut DKA cases by 76% in users who respond to alerts. These devices don’t just track sugar-they track ketones too. When ketones rise, you get an alert. People who use them say they call 911 or head to the ER within 30 minutes of the first warning. That’s the difference between a hospital stay and a death sentence.There’s even a new AI tool, DiaMonTech AG’s DKA Risk Score, that predicts DKA 12 hours before it happens by analyzing glucose trends. It’s being integrated into future versions of insulin pump systems. This isn’t science fiction-it’s already in use in some clinics.

Why People Delay: The Real Barrier to Survival
The biggest problem isn’t lack of treatment. It’s lack of recognition. A survey of over 1,200 people with diabetes found that 68% waited more than six hours before seeking help. Why? “I didn’t think it was serious.” “I thought it was just the flu.” “I didn’t want to go to the hospital.”Emergency rooms misdiagnose DKA as gastroenteritis in 18% of adult cases. That’s dangerous. If you’re vomiting, have abdominal pain, and have diabetes-DKA is the first thing they should check. Not a stomach bug. Not food poisoning. DKA.
Cost is another silent killer. The average monthly insulin cost in the U.S. is $374. People ration insulin because they can’t afford it. One in four people with type 1 diabetes has had DKA at least once-and nearly a third say it was because they skipped doses to save money. That’s not a medical issue. That’s a systemic failure.
What You Should Do Right Now
If you have diabetes, here’s what you need to do today:- Keep ketone strips or a blood ketone meter at home. Check ketones if your blood sugar is over 240 mg/dL for two readings in a row.
- If ketones are moderate or high, call your doctor or go to the ER. Don’t wait.
- If you’re on an insulin pump, have a backup plan for illness. Switch to injections if you’re sick.
- Teach your family what the warning signs are. The fruity breath, the deep breathing, the confusion-they’re not normal.
- If you’re on an SGLT2 inhibitor, know that you can get DKA even with normal glucose. Check ketones if you feel unwell.
DKA is preventable. It’s treatable. But only if you act fast. Every hour you wait increases your risk of death by 15%. You don’t need to be a doctor to save a life-you just need to know the signs and trust your gut.
Can you have diabetic ketoacidosis with normal blood sugar?
Yes. This is called euglycemic DKA and happens in about 10% of cases. It’s most common in people taking SGLT2 inhibitors like Jardiance or Farxiga, even if they have type 1 diabetes. Blood sugar may be below 250 mg/dL, but ketones are still high and blood is acidic. If you’re on one of these medications and feel sick, vomiting, or breathing deeply, check your ketones-even if your glucose looks normal.
Is diabetic ketoacidosis only for people with type 1 diabetes?
No. While 80% of DKA cases occur in type 1 diabetes, it can also happen in type 2 diabetes, especially during serious illness, infection, or if insulin therapy is stopped. People with type 2 who are insulin-deficient-often due to long-term disease progression or stress-are at risk. It’s less common, but just as dangerous.
How long does hospital treatment for DKA usually take?
Most people stay in the hospital for 2.5 to 4 days. But it depends on how bad it was when they arrived. If your blood pH was above 7.0, you might be discharged in 2 days. If it was below 7.0, you could need 4 or more days. Treatment continues until your ketones drop below 0.6 mmol/L, your bicarbonate is above 18 mmol/L, and your pH is back above 7.3 on two checks.
Can you treat DKA at home?
No. DKA is a medical emergency. Home treatment with extra insulin and fluids is not safe and can delay critical care. Even if you feel better after giving extra insulin, you still need hospital monitoring for electrolyte imbalances, brain swelling risk, and to find the root cause. Delaying hospital care increases your risk of death by 15% per hour.
What’s the biggest mistake people make with DKA?
Waiting too long to seek help. Many people think vomiting and fatigue are just the flu. Others don’t check ketones because their blood sugar isn’t sky-high. Some skip insulin because they can’t afford it. The biggest mistake is assuming it will get better on its own. DKA doesn’t resolve without medical intervention. Recognizing the signs early and going to the ER immediately is the only way to survive it.



Nicole Ziegler
November 19, 2025 AT 15:35Just checked my ketone strips after my BG hit 280... yikes. 🚨 Had no idea fruity breath = emergency. Thanks for this. I’m keeping strips in my purse now. 😅
Bharat Alasandi
November 20, 2025 AT 04:51Bro, this is life-saving info. SGLT2 inhibitors are sneaky AF-my cousin got euglycemic DKA and they thought it was gastro till his ketones hit 4.8. He’s lucky he made it. If you’re on Farxiga or Jardiance and feel off? Check ketones. No excuses. Insulin isn’t optional. 💪
Kristi Bennardo
November 20, 2025 AT 21:18This post is dangerously irresponsible. You’re normalizing a lethal metabolic crisis as if it’s a blog post about coffee. People are DYING because they’re being told to ‘trust their gut’ instead of calling 911 immediately. This is not a lifestyle tip. It’s a public health failure. Hospitals need to be mandated to screen every vomiting diabetic for DKA-not leave it to ‘awareness.’
Shiv Karan Singh
November 21, 2025 AT 02:18lol u think DKA is rare? my cousin in delhi got it after skipping insulin for 3 days cause he was 'too lazy' to buy it. he died in the ambulance. also... why are u all acting like this is new info? we've known this since the 80s. also... u said 'fruity breath' like its some magic sign. its acetone. its chemistry. learn it.
Ravi boy
November 21, 2025 AT 17:30so i got this from india too... my uncle had dka and they thought it was food poisining for 2 days... he was in icu for 5 days... now he uses cgms and checks ketones like its his job... also i typoed dka like 3 times while typing this lmao
Matthew Peters
November 22, 2025 AT 16:00Okay but the part about cerebral edema in kids? That hit me like a truck. I’ve got a 9-year-old with T1D and I’ve been checking her ketones every time her glucose goes above 240… but I had no idea brain swelling could happen *during treatment*. That’s terrifying. I’m printing this out and taping it to the fridge. Every. Single. Day.
Jeremy Samuel
November 23, 2025 AT 04:50wait so u can get dka with normal sugar? that sounds like a scam. i mean like... if the sugar is normal why even bother? maybe its just a marketing ploy by dexcom to sell more sensors. also i think u spelled 'ketones' wrong in the title. just sayin'
Destiny Annamaria
November 24, 2025 AT 08:21OMG I just told my whole family this last night. My little sister is pre-diabetic and she thought ‘diabetes’ meant ‘no sugar’-like she can eat cake if she takes insulin. I showed her the fruity breath thing and she said ‘eww that’s gross’ and now she checks her glucose after pizza. Progress! 🎉
Alyssa Torres
November 24, 2025 AT 08:39I’ve been a nurse for 12 years and I still get chills reading this. The most heartbreaking part? The people who ration insulin. One woman came in with a 3-day-old insulin bottle she’d been stretching out… she didn’t know she could get it for $35 a month through patient assistance. We need more outreach. Not just awareness-access. This isn’t about willpower. It’s about justice.
Summer Joy
November 25, 2025 AT 13:52so let me get this straight-people are dying because they’re ‘too lazy’ to check ketones? and you think the solution is to ‘trust your gut’? what a load of bs. this isn’t a pep talk, it’s a cry for help from a broken system. and now you’re making it sound like it’s the patient’s fault for not being ‘aware.’ #toxicpositivity
Aruna Urban Planner
November 26, 2025 AT 16:03DKA is a perfect storm of biology, access, and human behavior. The science is clear, but the social infrastructure isn’t. In rural India, a child with T1D might not have access to a glucometer, let alone a CGM. We need low-cost ketone strips, community health worker training, and insulin subsidies-not just individual vigilance. Awareness is a start, but equity is the cure.