Gallstone Risk Calculator
Assess Your Gallstone Risk
Enter your health information to calculate your risk of developing cholesterol gallstones based on the latest medical research.
Key Takeaways
- Elevated blood cholesterol raises the chance of forming cholesterol‑based gallstones.
- Obesity, diabetes and a high‑fat diet amplify that risk.
- Managing cholesterol through diet, exercise and medication can lower gallstone incidence.
- Two main stone types exist: cholesterol gallstones and pigment gallstones, each with different causes.
- Regular check‑ups and blood‑lipid monitoring help catch problems early.
What are Gallstones?
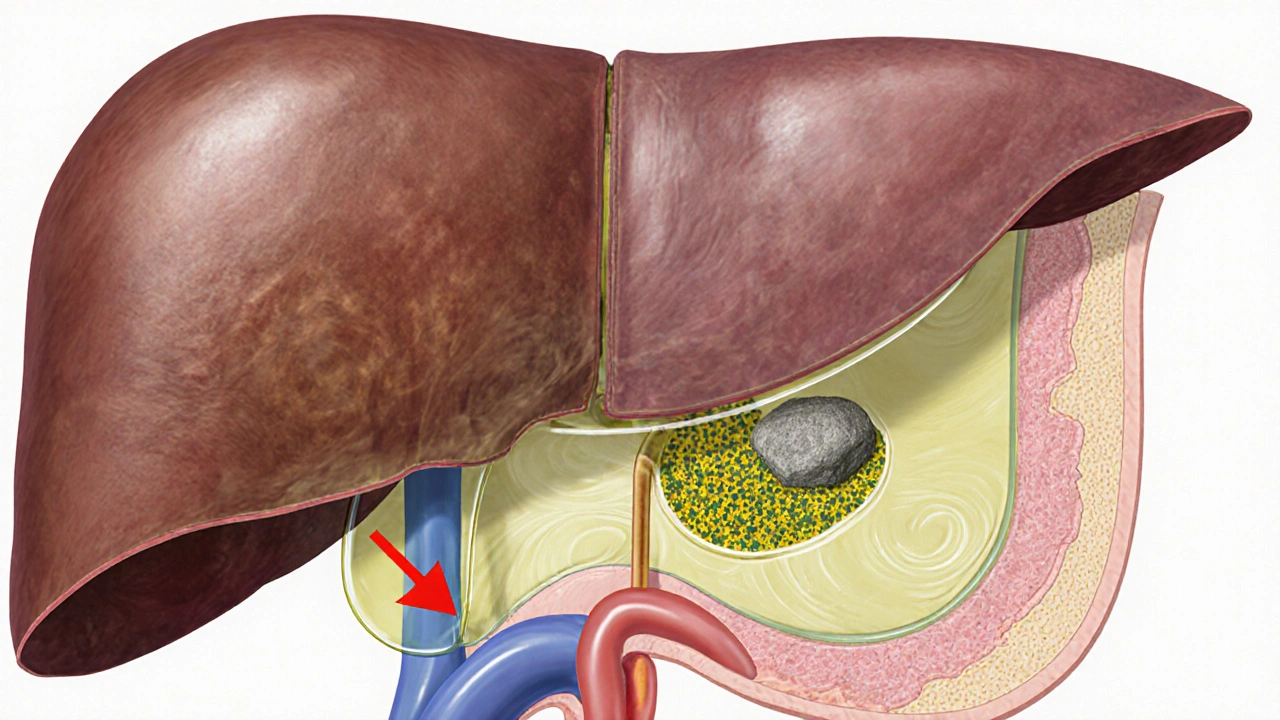
Gallstones are solid particles that form in the gallbladder, a small organ beneath the liver that stores bile. When bile becomes supersaturated with certain substances, those substances crystallise and grow into stones. People can have a single stone or dozens, and stones may stay hidden or cause severe pain if they block the bile ducts.
How Cholesterol Enters the Picture
Cholesterol is a waxy lipid carried in the bloodstream. It’s essential for building cell membranes and making hormones, but too much circulates in the blood, a condition known as high blood cholesterol. The liver regulates cholesterol levels by producing, storing, and secreting it into bile. When blood cholesterol is high, the liver often secretes more cholesterol into bile, raising the bile’s cholesterol concentration.
This excess cholesterol can precipitate, forming the core of cholesterol gallstones. The process is called cholesterol supersaturation: bile can’t keep the extra cholesterol dissolved, so it crystallises and eventually aggregates into stones.

Types of Gallstones and Their Links to Cholesterol
There are two major families of gallstones:
- Cholesterol gallstones are made primarily of cholesterol crystals mixed with bilirubin and calcium salts.
- Pigment gallstones consist mainly of calcium bilirubinate, often linked to hemolysis, liver disease, or infection.
High blood cholesterol directly fuels the formation of cholesterol gallstones, while pigment stones arise from different pathways unrelated to lipid levels.
Key Biological Players
Understanding the link requires a quick tour of the organs and substances involved:
- Liver produces bile, stores excess cholesterol, and regulates lipid metabolism.
- Bile is a digestive fluid containing bile acids, cholesterol, phospholipids, and bilirubin.
- Cholesterol metabolism refers to the body’s processes that synthesise, absorb, transport, and excrete cholesterol.
If any of these components become imbalanced-especially an overload of cholesterol in bile-the risk of stone formation spikes.
Risk Factors that Amplify the Cholesterol‑Stone Connection
While high blood cholesterol is a primary driver, several lifestyle and health conditions magnify the danger:
- Obesity raises serum cholesterol and alters bile composition, making stones more likely.
- Diabetes often co‑occurs with dyslipidaemia, and high insulin levels can increase cholesterol secretion into bile.
- High‑fat, low‑fiber diet supplies excess dietary cholesterol and reduces bile‑acid recycling, both of which promote supersaturation.
- Rapid weight loss (e.g., after bariatric surgery) can cause the liver to release stored cholesterol, temporarily spiking stone risk.
Prevention Strategies: Lowering Blood Cholesterol to Protect the Gallbladder
Because the cholesterol‑stone pathway is modifiable, several evidence‑based steps can keep both blood lipids and gallstone risk in check.
- Adopt a heart‑healthy diet. Emphasise whole grains, legumes, fruits, and vegetables. Limit saturated fats (found in red meat, butter) and replace them with polyunsaturated fats (olive oil, nuts). This approach can reduce LDL‑cholesterol by 5‑10% on average.
- Maintain a healthy weight. Losing 5-10% of body weight improves lipid profiles and lowers bile‑cholesterol concentration.
- Exercise regularly. Aerobic activity for at least 150 minutes per week modestly raises HDL‑cholesterol and improves insulin sensitivity, indirectly reducing gallstone risk.
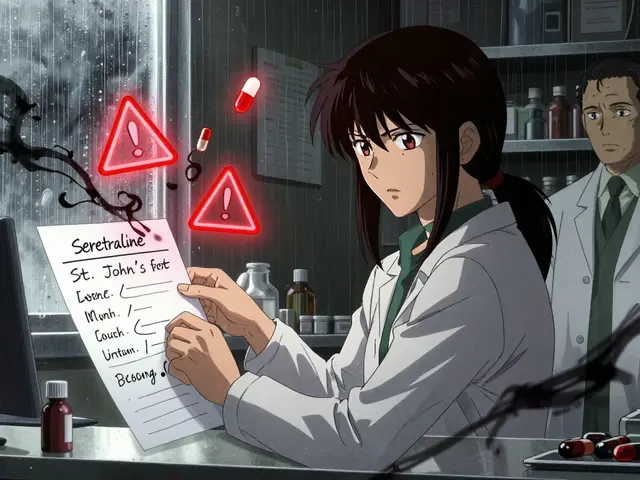
- Consider medication when lifestyle isn’t enough. Statins lower LDL‑cholesterol and have been associated with a modest decrease in cholesterol gallstone formation in several cohort studies.
- Monitor blood lipid levels. Annual lipid panels help catch rising cholesterol early, allowing timely intervention.
When to Seek Medical Attention
If you experience sudden, intense right‑upper‑abdominal pain lasting more than a few hours, especially after a fatty meal, it could be a gallstone blocking the cystic duct (biliary colic). Accompanying symptoms may include nausea, vomiting, fever, or jaundice. In such cases, a doctor may order an ultrasound, blood tests, and possibly a lipid panel to assess underlying risk factors.
Early detection of high cholesterol gives your physician a chance to prescribe statins or dietary adjustments before stones cause complications.
Comparing Cholesterol and Pigment Gallstones
| Feature | Cholesterol Gallstones | Pigment Gallstones |
|---|---|---|
| Primary Composition | Cholesterol crystals, bilirubin, calcium salts | Calcium bilirubinate, polymerised bilirubin |
| Typical Color | Yellow‑green | Black or brown |
| Associated Risk Factors | High blood cholesterol, obesity, rapid weight loss, female sex, age >40 | Hemolytic anemia, liver cirrhosis, infections, chronic alcoholism |
| Prevention Focus | Lipid management, diet, weight control | Treat underlying hemolysis or liver disease |
| Response to Statins | Potential reduction in incidence | No direct effect |
Practical Checklist for Reducing Your Gallstone Risk
- Get a fasting lipid panel at least once a year.
- Limit saturated fat to <10% of daily calories.
- Eat at least 25g of soluble fiber daily (oats, beans, apples).
- Maintain a BMI between 18.5 and 24.9.
- Exercise 30minutes a day, 5days a week.
- Ask your doctor about statin therapy if LDL‑C stays above 130mg/dL despite lifestyle changes.
- Know the warning signs of biliary colic and seek care promptly.
Frequently Asked Questions
Can high cholesterol cause gallstones even if I’m slim?
Yes. While obesity increases risk, the core mechanism is cholesterol supersaturation in bile. People with genetically high LDL‑C can develop cholesterol gallstones despite a normal weight.
Do statins really lower the chance of gallstones?
Observational studies suggest statins reduce cholesterol gallstone formation by about 10‑15% because they lower circulating LDL‑C, which translates to less cholesterol entering bile.
Is a low‑fat diet enough to prevent stones?
A low‑fat diet helps, but you also need enough fiber and regular physical activity. The combination controls both blood lipids and bile‑acid circulation.
How fast can gallstones form after rapid weight loss?
Stones can appear within weeks of a drastic calorie cut or bariatric surgery because the liver releases stored cholesterol into bile during the catabolic phase.
Should I get an ultrasound if my cholesterol is high but I have no symptoms?
Routine screening for gallstones isn’t necessary unless you have additional risk factors (obesity, diabetes, family history). Discuss with your physician to decide.
Understanding how high blood cholesterol fuels cholesterol gallstone formation empowers you to act. By keeping lipid levels in check, you protect not only your heart but also your gallbladder.


Dorothy Anne
October 12, 2025 AT 03:06Whoa, that whole cholesterol‑gallstone connection is a real eye‑opener! 🎉 Keep an eye on those lipid panels and stay active – the gallbladder will thank you. Even small diet tweaks can make a big difference, so keep that momentum going!
Sharon Bruce
October 12, 2025 AT 08:40All this medical mumbo‑jumbo proves why America needs top‑notch health education. 🇺🇸 Let’s push for better screenings and nutrition info.
True Bryant
October 12, 2025 AT 14:13From a pathophysiological standpoint, hypercholesterolemia precipitates supersaturation of bile, precipitating cholesterol nucleation – a classic cascade of dyslipidemia‑induced lithogenesis. The interplay of hepatic cholesterol secretion and impaired bile acid recirculation is a textbook example of metabolic dysregulation. Moreover, the epidemiological data unequivocally correlate LDL spikes with increased gallstone prevalence, underscoring a causal nexus. One must also consider the ancillary role of insulin resistance, which exacerbates hepatic cholesterol output. In short, the moral imperative is clear: regulate your lipid profile or risk biliary obstruction.
Danielle Greco
October 12, 2025 AT 19:46Grammar check: the article is spot on, but watch the pluralization – “risk factors” should stay plural when you list them. Also, love the colorful analogies! 🌈 Keep the science clear and the sentences vivid.
Linda van der Weide
October 13, 2025 AT 01:20Philosophically, our bodies echo the ancient balance of excess and deficiency. When cholesterol overwhelms bile, it’s a microcosm of societal overindulgence. One could argue the gallbladder is a silent sentinel, warning us of our over‑rich diets. The piece neatly ties biochemical pathways to daily habits – a reminder that health is both science and ethic.
Philippa Berry Smith
October 13, 2025 AT 06:53Alright, let’s peel back the layers of this so‑called "cholesterol‑gallstone" conspiracy. First, the pharmaceutical industry loves to paint high‑fat diets as the villain, because that keeps us buying their miracle statins. Second, the whole "supersaturation" narrative is just a fancy way of saying "your liver is dumping excess cholesterol into your bile because it’s being over‑fed by processed foods" – a fact that big agribusinesses hide behind vague health guidelines. Third, the studies cited rarely disclose funding sources; you can bet the sugar lobby had a hand in softening the blow about diet. Fourth, the calculator’s algorithm seems to over‑weight LDL – a classic move to push people toward prescription meds rather than lifestyle change.
Fifth, notice how the risk levels are split into neat boxes: low, medium, high. Real life is messier – many people with normal cholesterol still get gallstones due to genetic quirks, yet they’re told to “watch your diet”. Sixth, the article mentions rapid weight loss after bariatric surgery as a risk – that’s a direct jab at cutting‑edge weight‑loss clinics that market themselves as safe, while the truth is they may inadvertently increase gallstone formation by flooding the liver with stored cholesterol.
Seventh, the recommendation to “consider medication like statins” is vague, but it’s a nod to pharma: here’s a cue to ask your doctor for a prescription. Eighth, the piece glosses over the fact that cholesterol gallstones are just one type; pigment stones, often linked to infections and hemolysis, are ignored – an omission that keeps the narrative focused on lipid control, again feeding drug sales.
Ninth, the “heart‑healthy diet” suggestion is basically “eat more nuts and fish”, which conveniently aligns with nut and fish industry lobbying. Tenth, the article claims “annual lipid panels” catch problems early, but the CDC’s own data shows that over 70% of adults never get regular screenings, so the system is set up to miss the majority while still selling diagnostic tests. Eleventh, the “structured exercise plan” is a vague promise that gyms love to market as a cure‑all, even though sedentary lifestyles are entrenched in workplace culture funded by corporate interests.
Twelfth, the piece briefly mentions “statins may reduce gallstone incidence” – a claim that comes from a handful of small studies funded by the big pharma giants. Thirteenth, the overall tone is reassuring, but the reality is that many patients still suffer gallstone attacks despite following all the advice, indicating a deeper flaw in the oversimplified model presented.
Fourteenth, even the graphics in the article are designed with soothing blues and greens, a classic tactic to lull the reader into complacency while the underlying message pushes a medical‑industrial agenda. Fifteenth, the true takeaway? Our bodies are being weaponized by a network of food manufacturers, pharmaceutical companies, and medical device firms, all profiting off the fear of “cholesterol‑related gallstones”. The only real antidote is informed skepticism, a whole‑food diet, and questioning every “expert” who tells you to swallow a pill rather than change your plate.
Joel Ouedraogo
October 13, 2025 AT 12:26While conspiratorial narratives abound, the biochemical reality remains: excess hepatic cholesterol inevitably saturates bile, fostering nucleation. Ignoring the mechanistic link does not diminish its clinical relevance, and policy should reflect the empirical evidence rather than speculation.
Beth Lyon
October 13, 2025 AT 18:00i think im more concern with the diet side
Nondumiso Sotsaka
October 13, 2025 AT 23:33Great summary! 🙌 Keep sharing these practical tips – they really help people take control of their health. 🌟
Ashley Allen
October 14, 2025 AT 05:06Keep it concise: monitor lipids, stay active, and eat balanced meals.
Megan C.
October 14, 2025 AT 10:40Frankly, the article oversimplifies the moral responsibility of individuals while ignoring systemic food policies. People deserved better guidance than vague “watch your diet” advice.
Greg McKinney
October 14, 2025 AT 16:13Well, maybe cholesterol isn’t the only villain here. Genetics, gut microbiota, and even stress can play a role – don’t put all the blame on butter.
Dawna Rand
October 14, 2025 AT 21:46Thanks for the thorough breakdown! 🎉 It’s amazing how cultural food choices intersect with medical advice. 🍎🌍 Let’s keep spreading awareness worldwide.
Effie Chen
October 15, 2025 AT 03:20Interesting points! I’m curious how dietary patterns in different regions affect gallstone composition. 🌏 Could there be a link between traditional cuisines and stone type prevalence?
rohit kulkarni
October 15, 2025 AT 08:53In summation, the pathophysiological cascade-excessive hepatic cholesterol secretion → bile supersaturation → nucleation of cholesterol crystals-constitutes an incontrovertible mechanistic pathway; thus, therapeutic interventions must target each juncture. Moreover, the epidemiological correlations affirm causality, rendering the argument indisputable.
RONEY AHAMED
October 15, 2025 AT 14:26Hey folks, keep it simple: check your cholesterol, move a bit, and eat more veggies. You’ve got this!
emma but call me ulfi
October 15, 2025 AT 20:00Let’s stay calm and share reliable information. Everyone can make small changes for better health.
George Gritzalas
October 16, 2025 AT 01:33Wow, such a *masterpiece* of medical prose-if only the grammar were as perfect as the cholesterol stats. 🙄