Managing multiple pharmacies and prescribers isn’t just about keeping shelves stocked or prescriptions filled. For seniors on five or more medications, a misstep between pharmacies or prescribers can lead to dangerous drug interactions, duplicate therapies, or missed refills. The stakes are high, especially when patients juggle specialists, primary care doctors, and multiple pickup locations. Without a unified system, errors happen - and they’re often invisible until it’s too late.
Why Multi-Location Pharmacy Management Matters for Seniors
Seniors are the largest users of prescription medications in Australia and the U.S. On average, those over 65 take 4 to 6 prescriptions daily. Some take more. When they visit multiple doctors - a cardiologist, a neurologist, a pain specialist - each may prescribe without knowing what the others have ordered. Add in multiple pharmacies, and the risk of duplication, contraindications, or dosage errors skyrockets.
Without centralized oversight, a senior might get two different prescriptions for the same blood thinner from two doctors, filled at two different pharmacies. One pharmacy doesn’t know about the other. The pharmacist doesn’t catch it. The patient takes both. Result? Internal bleeding. Emergency room visit. Hospitalization.
According to the Pharmacy Quality Alliance, multi-location pharmacy chains using centralized systems saw a 29% drop in duplicate therapy incidents. That’s not a number. That’s lives saved.
The Core Problem: Fragmented Systems
Many small pharmacies still run on standalone software. Each location has its own database. Patient records don’t talk to each other. Prescriptions don’t sync. Inventory doesn’t move. Prescribers call one pharmacy, then another, and get conflicting answers.
That’s the old way. And it’s dangerous.
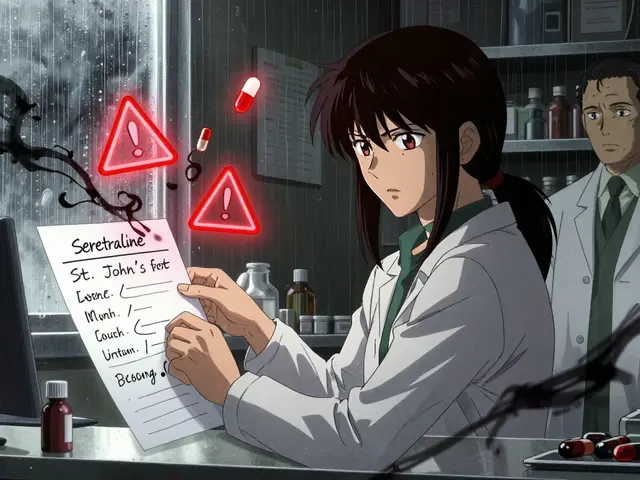
Without a central drug file, names vary. One pharmacy calls it “Metoprolol Tartrate,” another calls it “Toprol.” A senior’s file shows both. The system doesn’t recognize they’re the same drug. The pharmacist misses the conflict. The patient gets two doses.
Studies show 1.3% of prescriptions in fragmented systems contain errors due to inconsistent drug naming. That might sound small. But in a chain of 10 pharmacies filling 20,000 prescriptions a month, that’s 260 errors. Some of those are fatal.
How Centralized Systems Fix This
Modern pharmacy management systems like EnterpriseRx by McKesson, PrimeRx by PioneerRX, and Datascan’s Central Store Management unify everything under one roof - literally.
Here’s how they work:
- All pharmacies share a single, updated drug database with standardized names, NDC codes, and dosages.
- Prescriptions from any prescriber are instantly visible across all locations.
- Inventory moves between stores automatically based on demand - no more running out of insulin at one pharmacy while another has 20 extra bottles.
- Drug interaction checks run in real time across the entire network, not just one store.
These systems use AES-256 encryption to protect data. They sync daily - or even in real time - so if a prescriber changes a dose at 9 a.m. in one city, the change appears at 9:02 a.m. in another.
One chain in Melbourne saw a 44% drop in controlled substance discrepancies after using Datascan’s Watchdog feature. That’s because the system flags unusual patterns - like a patient picking up oxycodone from three different locations in one week - without staff having to log into each system separately.

Choosing the Right System: Key Features to Look For
Not all systems are built the same. Here’s what actually matters:
1. Universal Drug File
Must include all brand and generic names, NDC codes, and therapeutic equivalents. No exceptions. If a drug name varies between stores, the system fails.
2. Real-Time Patient Profile Access
Pharmacists need to see every prescription a patient has filled - anywhere in the chain - before filling a new one. PrimeRx lets patients pick a “preferred location” and auto-transfers prescriptions. That’s huge for seniors who travel or move between family homes.
3. Automated Inventory Balancing
Datarithm’s system cuts inventory-related errors by 28% by recommending store-to-store transfers and automatic returns to wholesalers. No more expired meds. No more shortages.
4. Clinical Service Integration
Many seniors need flu shots, diabetes counseling, or medication reviews. DocStation lets pharmacies bill for these services across all locations. One chain increased immunization revenue by 63% after implementing it.
5. AI-Powered Safety Alerts
EnterpriseRx’s new integration with Epic EHR lets prescribers send real-time updates directly into the pharmacy system. AI Watchdog 2.0 (launched Jan 2024) spots potential diversion or abuse patterns with 92.4% accuracy. That’s not sci-fi. That’s today’s standard.
Cost and Implementation: What to Expect
Systems aren’t cheap. But the cost of not using one is higher.
- Liberty Software’s PharmacyOne: Starts at $299 per location/month. Good for small chains (under 5 stores).
- EnterpriseRx: $450 per location/month, but drops to $325 for 15+ locations. Best for chains with complex clinical needs.
- PrimeRx Pro: Competitive pricing, best for patient mobility and inventory control.
Implementation takes 8-12 weeks. Staff need 16 hours of training per technician, 24 hours per pharmacist. Chains that use vendor-certified trainers see 12% higher adoption rates.
Expect data migration headaches. 27% of chains report prescription history errors during the switch. Plan for manual verification of 15% of active patient files. It’s tedious. But necessary.
The Hub-and-Spoke Model: The Gold Standard
The best systems don’t take control away from local pharmacists. They empower them.
The “hub-and-spoke” model works like this:
- The hub (central office) manages drug files, pricing, inventory transfers, and compliance.
- The spokes (local pharmacies) handle clinical decisions - verifying prescriptions, counseling patients, catching red flags.
A University of California study found this approach reduced medication errors by 38% compared to fully centralized systems where clinical decisions were made remotely.
Why? Because the pharmacist at the counter knows the patient’s habits, their memory issues, their family support. The system gives them the data. They use their judgment.
What Happens Without a Central System?
Chains without centralized management have higher error rates - and higher costs.
- 23% report billing discrepancies between locations.
- 17% of errors come from inconsistent drug naming.
- 12% of medication errors happen during transfers when local pharmacists don’t verify incoming prescriptions.
And it’s getting worse. CMS now requires multi-location pharmacies to track cross-location errors for Medicare Part D compliance. If you can’t prove you’re doing it, you lose reimbursement.
By 2027, the Pharmacy Quality Alliance predicts centralized systems will be mandatory for any chain with three or more locations.
What’s Next: AI, Blockchain, and FHIR
The future is here.
AI is now spotting opioid diversion before it becomes a crisis. Blockchain pilots have cut prescription fraud by 67% in multi-location trials. And FHIR API compliance - required by CMS in 2025 - will force all systems to talk to hospital EHRs in real time.
But here’s the catch: 63% of current systems aren’t ready. Upgrades will cost $200,000+. Smaller vendors won’t survive. If you’re still using a system from 2018, you’re already behind.
Final Advice: Start Now, Not Later
If you manage multiple pharmacies or work with seniors on multiple medications, don’t wait for a mistake to force your hand.
Start by mapping your current workflow. Where do prescriptions get lost? Where do drug names conflict? Where do patients get confused about pickup locations?
Then talk to vendors. Ask for live demos. Watch how the system handles a patient with 8 prescriptions, 3 prescribers, and 2 pharmacies. See if it flags a potential interaction between a blood thinner and an NSAID. See if it shows you where that prescription was filled last month.
Don’t buy based on price alone. Buy based on safety.
Because when it comes to senior medications, the cost of inaction isn’t measured in dollars. It’s measured in hospital beds, ER visits, and lives.
Can one pharmacy system manage 20+ locations?
Yes. Systems like Datascan’s Central Store Management and EnterpriseRx support unlimited locations. Data syncs daily or in real time, and all pharmacies share the same drug database, pricing, and patient records. There’s no technical cap - only licensing and training considerations.
How do I prevent duplicate prescriptions from different doctors?
Use a system with real-time, centralized patient profiles. When a new prescription is entered, the system checks all other active prescriptions across every location. If a duplicate or interaction is found, it alerts the pharmacist before filling. EnterpriseRx and PrimeRx both do this automatically.
Do I need to train all staff again if I switch systems?
Yes, but it’s worth it. Plan for 16 hours per technician and 24 hours per pharmacist. Chains that use vendor-certified trainers report 12% higher adoption. Don’t rely on internal staff alone - the learning curve is steep, and mistakes during transition can be dangerous.
Is cloud-based better than on-site software?
Yes. Cloud-based systems offer 99.99% uptime, automatic updates, remote access for managers, and real-time syncing. On-site systems require hardware maintenance, manual updates, and often limit connectivity between locations. For multi-location chains, cloud is the only safe choice.
Can seniors pick up prescriptions at any location?
Yes - if the system supports it. PrimeRx and EnterpriseRx let patients designate a preferred pickup location and transfer prescriptions between any store in the chain. This is critical for seniors who travel between family homes or live in multiple cities.
What’s the biggest mistake pharmacies make when switching systems?
Skipping the data migration check. 27% of chains experience prescription history errors during the switch. Always manually verify 15% of active patient files after go-live. Don’t assume the system got it right. Double-check the high-risk meds - blood thinners, insulin, opioids.
Will this help with Medicare Part D compliance?
Yes. CMS now requires multi-location pharmacies to track and report cross-location prescription errors. Only centralized systems can provide the audit trail and error detection needed. Without one, you risk losing reimbursement.
Are there free or low-cost alternatives?
No. There are no reliable, compliant, safe free systems for multi-location pharmacies. Trying to use spreadsheets, email, or basic software creates dangerous gaps. The cost of a single medication error far exceeds the monthly fee of a professional system.


Katherine Blumhardt
December 26, 2025 AT 03:07Just had to refill my grandma’s blood thinner last week and the pharmacy had NO IDEA she got another script from the cardiologist 2 days ago. We almost lost her. This post? 100% needed. I’m screaming into the void but someone finally said it out loud.
sagar patel
December 27, 2025 AT 01:44Centralized systems reduce errors. Data sync prevents duplication. Standardized NDC codes eliminate naming conflicts. Implementation cost is minor compared to liability exposure. Case closed.
Bailey Adkison
December 27, 2025 AT 19:09So you’re telling me the solution to human error is more software? Brilliant. Next you’ll say AI will fix bad parenting. Let me guess - the vendor’s CEO drives a Tesla and owns a yacht. Meanwhile real pharmacists are drowning in paperwork while the system ‘syncs.’ I’ve seen this movie. It ends with a lawsuit and a shutdown.
Michael Dillon
December 29, 2025 AT 00:27Okay but have you tried PrimeRx? The inventory balancing is next level. My cousin works at a 7-store chain in Ohio and they went from running out of insulin every other Tuesday to having 3 extra bottles at every location. Also the AI alert that flagged a guy picking up oxycodone from 3 stores? Saved his life. And no, I don’t work for them. I just don’t want anyone’s grandma to bleed out because someone didn’t update a database.
Sophie Stallkind
December 30, 2025 AT 09:13Thank you for this comprehensive and meticulously researched piece. The statistical evidence presented, particularly the 29% reduction in duplicate therapy incidents and the 44% decline in controlled substance discrepancies, provides compelling justification for systemic investment. The hub-and-spoke model demonstrates a nuanced understanding of clinical autonomy and operational efficiency. I commend the author for emphasizing patient-centered safety over cost reduction.
Winni Victor
December 30, 2025 AT 10:12Ugh. Another ‘tech is the answer’ rant. You know what fixes this? Talking to people. Not databases. My aunt had 11 meds and her pharmacist knew her by name, her dog’s name, and that she hated grapefruit. The system didn’t know she was on vacation in Florida. The pharmacist did. You can’t code empathy. You just can’t.
Terry Free
December 31, 2025 AT 06:29AI Watchdog 2.0? Yeah right. That’s just a fancy way of saying ‘we’re replacing pharmacists with bots.’ And don’t get me started on ‘cloud-based is the only safe choice.’ My uncle’s pharmacy in rural Iowa still runs on Windows XP and a printer. They’ve never had a fatal error. Meanwhile, the fancy new system in Chicago crashed last month and 400 patients got wrong meds because the server ‘synced wrong.’
Lindsay Hensel
December 31, 2025 AT 22:31Thank you for this vital contribution. The hub-and-spoke model is not merely an operational framework - it is a philosophical recentering of care. Technology serves, it does not supplant. The pharmacist’s judgment, rooted in human connection, remains irreplaceable. I urge all stakeholders to prioritize dignity over automation. Lives are not data points.