What Exactly is a Boxed Warning?
Boxed Warning is the FDA's strongest safety alert for prescription drugs, appearing as a bordered section at the start of prescribing information. Introduced in 1979, these warnings highlight risks that could cause death or serious harm. Unlike regular warnings, boxed warnings require specific language about prevention, precautions, or use restrictions.
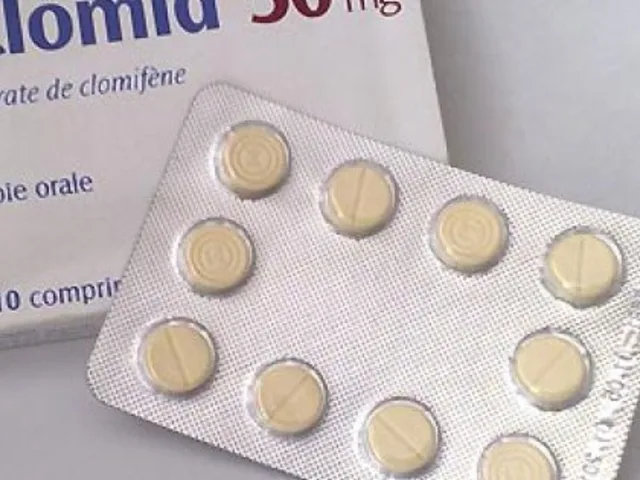
For example, the Clozaril warning now specifies myocarditis incidence rates, while Avandia's warning details heart attack risks in patients with existing heart disease. Each update reflects new evidence gathered from real-world use.
Why do these warnings exist? The FDA created them to ensure prescribers and patients are aware of life-threatening risks before using a medication. A 2015 study found that 32.7% of drugs approved between 2001 and 2010 received boxed warnings, showing how common they are for high-risk medications.
How Boxed Warnings Have Evolved Over Time
Early boxed warnings in the 1980s and 1990s were often vague. Take the antidepressant warning issued in 2004: it simply stated "increased risk of suicidal thinking and behavior" in children and adolescents. By 2006, the FDA expanded this to include young adults aged 18-24 and added specific monitoring requirements. This shift from general statements to precise details is now standard.
The Unituxin warning evolution shows this clearly. In 2017, the term "neuropathy" was replaced with "neurotoxicity" and specific discontinuation criteria were added for severe pain or nerve damage. This precision helps doctors act faster when issues arise.
Another example is Avandia. Its 2007 warning about heart attack risks led to market withdrawal in Europe, though it remains available in the U.S. with restrictions. This shows how boxed warnings directly influence treatment decisions and regulatory actions.
Where to Find Current Boxed Warning Updates
Tracking these changes requires knowing where to look. The FDA maintains three key resources:
- SrLC Database - Updated quarterly since January 2016, this searchable database tracks all label changes. The April-June 2025 report included updates to Clozaril's myocarditis monitoring requirements.
- MedWatch - The FDA's program for receiving adverse event reports. While MedWatch itself doesn't list warnings, it's the primary source for data that triggers updates.
- Drugs@FDA - This archive shows a drug's entire approval history, including when boxed warnings were first added or modified.
Pharmacists and clinicians also rely on quarterly summaries from the American Journal of Health-System Pharmacy. The April-June 2025 issue documented 17 boxed warning updates across 14 medications, including Clozaril's new myocarditis details.
Why Do Boxed Warnings Change?
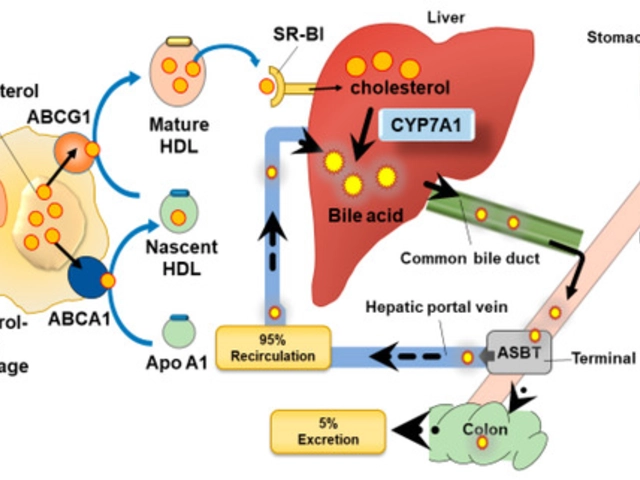
Changes happen for one simple reason: new data. When doctors report adverse events through MedWatch, the FDA analyzes this information to determine if a warning needs updating. For example, the Clozaril update in 2025 came from real-world data showing myocarditis incidence of 0.84 cases per 1,000 patient-years compared to 0.12 in non-clozapine antipsychotics.
Historically, the time between drug approval and a boxed warning has increased. A 2002 study found it took about 7 years, but by 2009, it was 11 years. This suggests either more complex safety issues or better post-marketing surveillance. However, the FDA's 2023 Modernization Act 2.0 aims to reduce this lag by using real-world evidence from electronic health records.
Challenges in Understanding and Applying Boxed Warnings
Despite their importance, healthcare providers often struggle with these warnings. A 2017 study showed only 43.6% of primary care physicians could correctly identify drugs with boxed warnings during clinical encounters. On physician networks like Sermo, 68.3% of 1,247 participants reported "frequent confusion" about applying warning criteria.
Compliance varies widely too. A 2021 study found warnings about rare catastrophic events (like liver failure) had 78.4% compliance, while those for common but less severe issues (like mild nausea) had only 42.1%. This "warning fatigue" means important alerts sometimes get ignored.
Yet, pharmacists report high value in these warnings. A 2023 survey found 89.7% of hospital pharmacists consider boxed warnings "essential for safe medication use," especially for high-risk drugs like clozapine and pimozide.

The Future of Boxed Warnings
The FDA's 2025-2027 Strategic Plan for Drug Safety focuses on "dynamic warning systems" that update in real-time using electronic health record data. Current systems have an 18-24 month lag between safety signals and warning updates, but new technology could cut this to days or weeks.
Industry analysts at Cortellis predict these changes will increase warning specificity by 60% while reducing length by 35%, addressing "warning fatigue." With 34.1% of Breakthrough Therapy drugs receiving boxed warnings compared to 22.7% of standard approvals, the FDA is clearly adapting to the pace of modern drug development.
As one FDA official put it in a 2024 internal assessment: "Boxed warnings are essential to medication safety, but they must evolve to stay relevant." For healthcare professionals, staying informed isn't just helpful-it's critical for protecting patients.
Frequently Asked Questions
How often do boxed warnings change?
The FDA issues 25-30 new or updated boxed warnings annually. For example, the April-June 2025 report documented 17 updates across 14 medications, including Clozaril's new myocarditis monitoring requirements. Changes typically occur when new safety data emerges from real-world use or clinical studies.
What's the difference between a boxed warning and a regular warning?
Boxed warnings are the FDA's strongest safety alerts, appearing in a bordered section at the start of prescribing information. They highlight risks that could cause death or serious harm. Regular warnings appear later in the document and address less severe issues, like common side effects or drug interactions. Only boxed warnings require specific language about prevention, precautions, or use restrictions.
How can I stay updated on new boxed warnings?
Subscribe to the FDA's Drug Safety-related Labeling Changes (SrLC) database updates, which are published quarterly. Pharmacists also rely on summaries from the American Journal of Health-System Pharmacy. For real-time alerts, set up email notifications through the FDA's MedWatch system for significant safety communications.
Why do some boxed warnings get removed?
Warnings are removed when new evidence shows the risk isn't as severe as previously thought. For example, Chantix's boxed warning about depression and suicidal thoughts was removed in 2016 after a large clinical trial of 8,144 participants found no significant difference in neuropsychiatric events compared to placebo. This shows the system adapts to accurate data.
What should I do if a medication's boxed warning changes?
First, review the updated prescribing information immediately. For high-risk drugs like Clozaril or pimozide, this may mean adjusting monitoring protocols or patient education. If the change affects your practice, consult with a pharmacist or specialist. Always document the update and any changes to treatment plans to ensure patient safety.

Mayank Dobhal
February 7, 2026 AT 10:24Boxed warnings are life-or-death. Always check SrLC.
Marcus Jackson
February 8, 2026 AT 01:30Actually, the FDA's SrLC database updates quarterly, but the real-time data comes from MedWatch. You need to cross-reference both.
Natasha Bhala
February 8, 2026 AT 03:44so true! i always check the ajhsp summaries too. they're super helpful for keeping up
Jesse Lord
February 8, 2026 AT 07:53good point about medwatch data. it's easy to overlook how much real-world evidence drives these updates
AMIT JINDAL
February 8, 2026 AT 16:40oh yeah totally! medwatch is where the real gold is but honestly sometimes it's overwhelming. like last month i was checking the clozaril updates and saw 0.84 cases per 1000 patient-years for myocarditis which is way higher than non-clozapine antipsychotics. also the new monitoring requirements are crucial. but here's the thing: most docs don't even know about the sr lc database updates. they just rely on their pharma reps who might not have the latest info. so yeah we need better systems but for now i just check the ajhsp journal every quarter. also check out this cool chart i made: 😎📊. wait, actually, the 2025 report showed 17 updates across 14 meds. clozaril's new myocarditis details are a big deal. but here's the kicker-pharmacists are way more aware than doctors. a 2023 survey said 89.7% of hospital pharmacists find boxed warnings essential. meanwhile, primary care docs only 43.6% can correctly identify them. that's why we need better training. also, the FDA's 2023 Modernization Act 2.0 is supposed to help, but it's still slow. real-world evidence from EHRs should speed things up. but until then, we're stuck checking quarterly reports. oh and the avandia warning? it led to market withdrawal in europe but stays in the us with restrictions. crazy how different countries handle this. anyway, the point is, stay updated. check sr lc, drugs@fda, medwatch. it's a pain but worth it. trust me, i've seen patients get hurt because of outdated warnings. so yeah, keep pushing for better systems. also, the cortellis analysts say future warnings will be 60% more specific and 35% shorter. that's good news for us. but until then, stay vigilant. check those updates every quarter. and if you see a new warning, act fast. don't wait for the next meeting. your patients depend on it.
Ritu Singh
February 9, 2026 AT 22:23It is imperative for all healthcare professionals to adhere to the latest FDA guidelines regarding boxed warnings. The April-June 2025 report clearly indicates significant updates to Clozaril's myocarditis monitoring requirements, necessitating immediate review of prescribing protocols.
Catherine Wybourne
February 10, 2026 AT 12:40oh sure, "imperative" - because we all have time to read every single update. Meanwhile, my clinic's pharmacy still uses the 2010 version of the manual. 🙄
Mark Harris
February 11, 2026 AT 07:46Love this topic! The FDA's new real-time systems are a game-changer. Imagine getting alerts the same day a new risk is found. No more waiting for quarterly reports!
Savannah Edwards
February 12, 2026 AT 01:13yeah totally! but honestly, even with real-time updates, the challenge is getting all the healthcare providers to actually check them. i've seen so many cases where a new boxed warning comes out but the doctors just keep prescribing the same way. like with avandia's heart attack risk-everyone knows it, but they still use it for patients with existing heart disease because they don't have alternatives. it's a real problem. also, the drug companies don't always make it easy to find the updated warnings. you have to dig through drugs@fda and medwatch to get the full picture. so yeah, we need better communication systems in place. maybe something like a simple mobile app that sends push notifications for all boxed warning changes? that would help so much.
Carol Woulfe
February 12, 2026 AT 08:00It is imperative to consider that the FDA may be utilizing boxed warnings as a mechanism to remove drugs from the market. Every new warning correlates with a decline in stock prices for the respective pharmaceutical companies. This suggests a coordinated effort between the FDA and large pharmaceutical entities to manipulate the market. Furthermore, the real-world evidence cited for these warnings is likely fabricated to maintain public trust. Such manipulation is detrimental to patient safety.
Gouris Patnaik
February 13, 2026 AT 11:20India's healthcare system is far more efficient than the US when it comes to tracking drug warnings. We have a centralized database that updates in real-time. The FDA's slow process is why so many patients suffer. Why don't they just copy our system?