What Is Tendinopathy, Really?
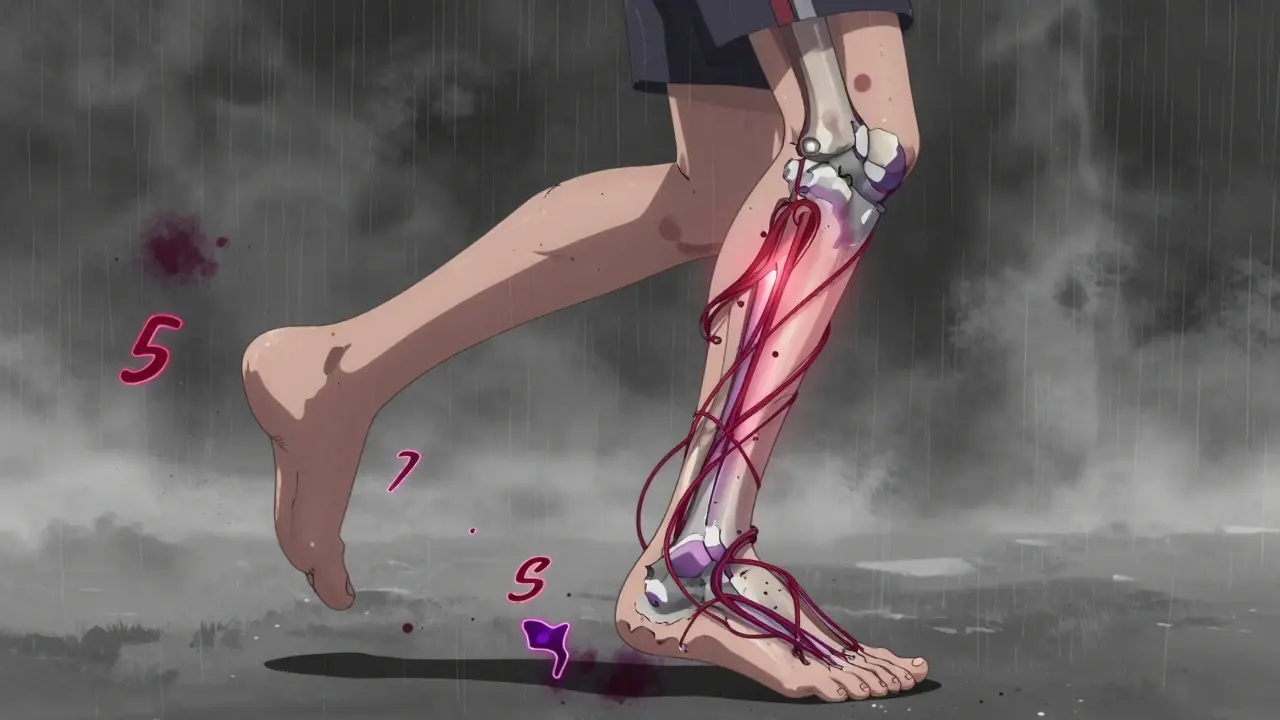
Tendinopathy isn’t just a sore tendon. It’s a failed healing response. The tendon, usually overloaded over time, starts breaking down instead of repairing. You feel pain when you move, stiffness in the morning, and maybe a lump you can feel along the tendon. It’s not inflammation like people think - that’s why anti-inflammatories often don’t help much. This is a structural problem. The collagen fibers inside the tendon get messy, weak, and disorganized. That’s why rest alone doesn’t fix it. You need to retrain the tissue.
It shows up in runners with achy heels (Achilles tendinopathy), jumpers with pain under the kneecap (patellar tendinopathy), and even office workers with shoulder pain from repetitive typing. About 30% of sports medicine visits involve this. And it’s not just athletes - anyone who suddenly increases activity, wears worn-out shoes, or has weak muscles around the joint is at risk.
Why Eccentric Training Works When Nothing Else Does
The breakthrough came in 1998 when Dr. Hakan Alfredson had patients with chronic Achilles pain do heel drops off a step - slowly lowering down, then using their good leg to come back up. No stretching. No ice. Just slow, heavy, controlled lowering. The results? Most patients got better. Not just less pain - actual tendon healing.
What’s happening? When you lower slowly under load, you’re giving the tendon a signal: rebuild stronger. The mechanical stress triggers tenocytes (tendon cells) to produce new, organized collagen. Ultrasound scans show the tendon thickens and straightens out after 8-12 weeks. That’s not magic. That’s biology.
For Achilles tendinopathy, the standard is Alfredson’s protocol: two feet on a step, rise up on both, then lower down slowly on the painful one - 3 sets of 15 reps, twice a day. Do it with the knee straight to target the calf muscle (gastrocnemius), then bend the knee to hit the deeper soleus. For patellar tendinopathy, single-leg decline squats on a 25-degree board are the gold standard. Lower slowly over 3-5 seconds, then push up with both legs.
Heavy Slow Resistance: The Quiet Contender
Turns out, eccentric training isn’t the only game in town. Heavy slow resistance (HSR) training - lifting weights slowly with control - does just as well, and for some people, it’s easier to stick with.
HSR uses 70% of your one-rep max. You lift the weight in 3 seconds, lower it in 3 seconds. Three sets of 15 reps, three times a week. No decline board needed. Just a dumbbell, a leg press, or a resistance band. In a 2015 study, HSR and eccentric training both improved VISA-A scores by 60-65%. But HSR had better adherence - 87% of people stuck with it versus 72% for eccentric. Why? Less pain at first.
For people who can’t tolerate the sharp pain of heel drops or decline squats, HSR is a smart alternative. It’s also easier to scale. You can start lighter and build up without needing special equipment. And if you’re already lifting weights, you can slot it right into your routine.
Isometric Exercises: The Quick Pain Fix
Need relief before a workout? Or just to get through the day? Isometric holds can give you immediate pain relief - within minutes.
For Achilles tendinopathy, stand on a step with your heels hanging off. Push up onto your toes and hold that position for 45 seconds. Do three holds, with 1-2 minutes rest between. For patellar tendinopathy, sit with your leg straight and squeeze your quad hard, holding for 45 seconds. Three times.
Studies show this cuts pain by 50% right away. It doesn’t fix the tendon long-term, but it’s a powerful tool to manage symptoms while you do your eccentric or HSR training. Many therapists now have patients do isometrics before their main exercise. It lowers pain enough to let them train harder without flaring up.

Injection Options: What Actually Helps - and What Doesn’t
Doctors still offer injections. But not all are created equal.
Corticosteroid shots give fast relief - 30-50% less pain in 2-4 weeks. Sounds great, right? But here’s the catch: after 6 months, 65% of people who got steroid shots needed more treatment. Only 35% of those who did eccentric training did. Steroids weaken the tendon over time. They mask the pain, but don’t heal the tissue. Use them only if you’re in severe pain and need a short-term window to start rehab.
Platelet-rich plasma (PRP) sounds fancy. You draw your own blood, spin it to concentrate platelets, then inject it into the tendon. The theory? Your body’s healing factors will jump-start repair. But the evidence? Weak. A 2020 review found PRP only beat placebo by 15-20% at 6 months. Not enough to justify the cost - often $500-$1,000 out of pocket. Most insurance won’t cover it.
Prolotherapy (sugar water injections) and dry needling have even less proof. Some people swear by them, but there’s no solid data backing their use for tendinopathy.
The bottom line: injections are not a cure. They’re a temporary bandage. Eccentric training, HSR, and isometrics are the real treatments. Injections might help you get started - but they won’t finish the job.
Why So Many People Fail - And How to Avoid It
Here’s the ugly truth: about 30% of people don’t improve with eccentric training. Why?
First, they don’t do it long enough. You need 12 weeks. Minimum. Most people give up after 4 or 5 because they don’t see results fast enough. Tendons heal slowly. That’s just how they work.
Second, they do it wrong. Too fast. Too light. Too few reps. A 2021 study found self-managed patients made errors 40% more often than those coached by a physical therapist. If you’re doing heel drops and your foot rolls inward, or your knee caves during squats, you’re not loading the tendon properly. You’re just hurting yourself more.
Third, they chase pain-free movement. That’s the wrong goal. You need to train through mild pain - 2 to 5 out of 10. That’s called ‘acceptable pain.’ If it’s 7 or above, or if pain lasts more than 24 hours, you’ve gone too far. But if you’re feeling nothing, you’re not challenging the tendon enough.
Use an app. The Tendon Rehab app (version 3.2, 2023) gives you video demos, timers, and reminders. People using it had 85% adherence. Those using paper sheets? Only 65%. Technology helps.
What Experts Are Saying Now
Dr. Jill Cook, a leading tendon researcher, says tendinopathy isn’t one thing - it’s a spectrum. She calls it the “tendon continuum.” At one end, you have reactive tendons - irritated but still healthy. At the other, you have degenerative tendons - frayed and worn. Treatment changes depending on where you are.
If you’re early stage (reactive), isometrics and light loading are best. If you’re chronic (degenerative), you need heavy, slow eccentric or HSR. One-size-fits-all doesn’t work.
Dr. Neal Barton points out another blind spot: we focus too much on the tendon and forget the whole body. Weak glutes? Tight hips? Poor ankle mobility? Those can overload the tendon in the first place. Fixing the tendon alone won’t help if the rest of your movement pattern is broken.
The future? Personalized rehab. Researchers are testing biomarkers - things like blood proteins or ultrasound texture - to predict who will respond to eccentric training and who needs something else. Early results show this could boost success rates by 40%.

Real People, Real Results
On Reddit’s r/PhysicalTherapy, one runner wrote: “I did 12 weeks of heel drops. First two weeks? Pure torture. I cried. But by week 8, I could jog without wincing. At 12 weeks, I ran a half-marathon. No pain. No shots. Just slow, painful, consistent work.”
Another, a volleyball player with patellar tendinopathy: “My coach made me do decline squats every day. I thought I’d never play again. After 3 months, my ultrasound showed the tendon looked normal. My coach said he’d never seen that before.”
But the ones who didn’t make it? They stopped too soon. Or did it once a week. Or tried to push through sharp pain. Or got a steroid shot and thought they were fixed.
What to Do Next
Start with isometrics. Do 3 holds of 45 seconds, twice a day, for 3-5 days. See if your pain drops. If it does, you’re a good candidate for rehab.
Then pick your path:
- For Achilles: Start Alfredson heel drops (3x15, twice daily). Use a step or curb. Lower slow. Rise with both legs.
- For patellar: Use a 25-degree decline board. Single-leg squats. 3x15 daily. If you don’t have a board, use a ramp or stack books under your toes.
- If it hurts too much: Switch to HSR. Use a leg press or dumbbells. 3x15, slow up and down, 3x a week.
Track your pain on a scale of 1-10 during and after each session. Keep a log. If pain stays under 5 during and doesn’t spike the next day, you’re on track.
See a physical therapist for at least one session to check your form. Even 30 minutes can prevent mistakes that cost you months.
Stick with it for 12 weeks. No shortcuts. No magic injections. Just consistency.
Final Thought
Tendinopathy isn’t a disease you cure. It’s a load management problem you fix. Your tendon isn’t broken - it’s just confused. Give it the right signal, over time, and it will rebuild. It’s slow. It’s hard. But it works. And it lasts.


Shae Chapman
December 31, 2025 AT 07:19Kunal Karakoti
December 31, 2025 AT 08:56Hayley Ash
January 2, 2026 AT 08:03kelly tracy
January 4, 2026 AT 02:47srishti Jain
January 4, 2026 AT 10:16Cheyenne Sims
January 4, 2026 AT 17:04Nadia Spira
January 5, 2026 AT 20:44Colin L
January 7, 2026 AT 17:51henry mateo
January 8, 2026 AT 11:01Kelly Gerrard
January 8, 2026 AT 17:03