When you’re older, your body doesn’t process medicine the same way it did when you were 30. That’s not just a guess-it’s science. A 75-year-old taking the same pill as a 45-year-old might end up with too much drug in their system, leading to dizziness, falls, confusion, or even hospitalization. The problem isn’t that the medicine is wrong. It’s that the dosage hasn’t been adjusted for an aging body.
Why Aging Changes How Drugs Work
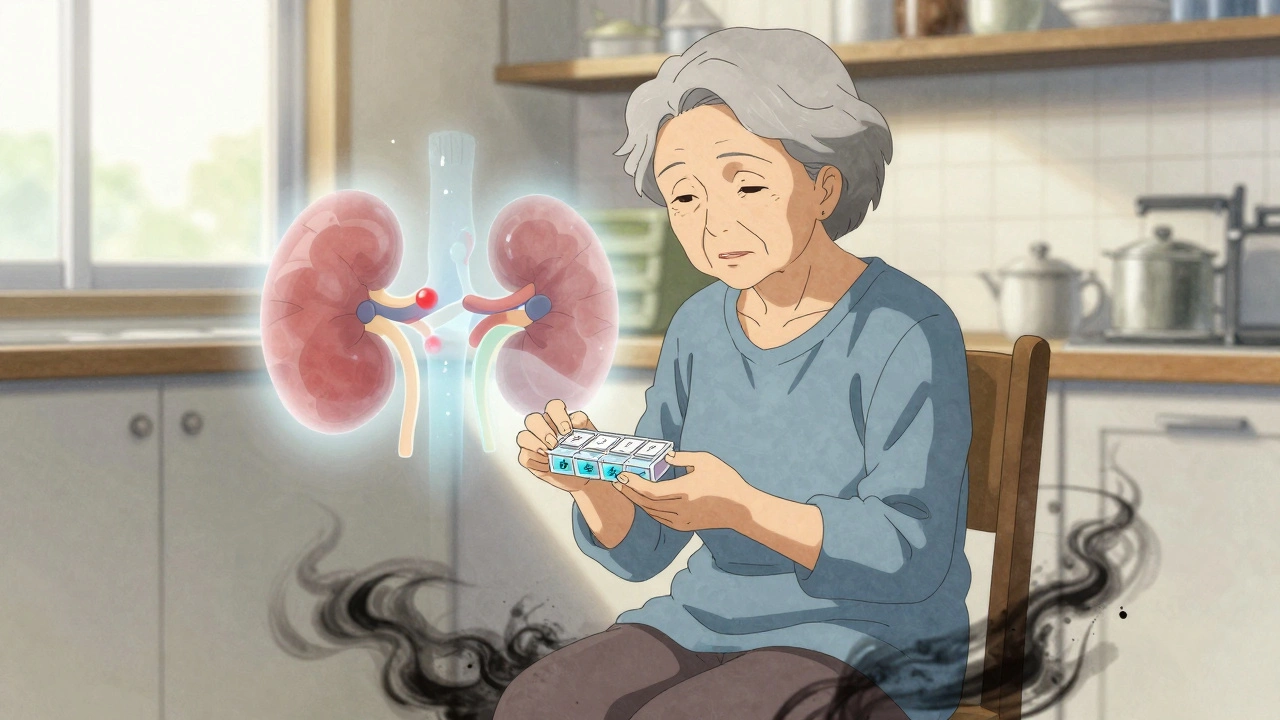
Your body changes as you get older. Your kidneys slow down. Your liver doesn’t break down drugs as quickly. Your body fat increases while muscle mass decreases. Even your stomach produces less acid. All of this affects how medicines are absorbed, distributed, metabolized, and cleared from your system.For example, many drugs are cleared by the kidneys. After age 30, kidney function drops by about 8 mL per minute every decade. By 70, it’s common for someone to have only half the kidney function they had in their 30s. If a drug like gabapentin or metformin is given at the standard adult dose, it builds up in the bloodstream. That’s why doctors now start with much lower doses for older adults.
Drugs that are broken down by the liver-like many antidepressants and painkillers-also become more potent in older people. The liver’s ability to process these drugs can drop by 30% to 50%. Even if you’re healthy, your liver isn’t working like it used to.
The Start Low, Go Slow Rule
This isn’t just a suggestion. It’s the golden rule of geriatric prescribing. The American Geriatrics Society has pushed this approach since the 1980s. It means starting with the lowest possible dose and waiting weeks, sometimes months, before increasing it.Take warfarin, a blood thinner. A typical adult dose might be 5 mg daily. For someone over 70, the starting dose is often 1 to 2 mg. Why? Because older adults are more sensitive to its effects. Too much can cause dangerous bleeding. Too little won’t protect against stroke. Finding the right balance takes time and careful monitoring.
The same goes for benzodiazepines like lorazepam. These are often prescribed for anxiety or sleep. But in older adults, they increase the risk of falls by 50%. The dose should be cut in half-or avoided entirely. The 2023 Beers Criteria® lists 30 classes of drugs that should be used with extreme caution-or not at all-in seniors.
How Doctors Calculate the Right Dose
There’s no one-size-fits-all formula, but there are trusted tools doctors use.One of the most common is the Cockcroft-Gault equation. It estimates how well your kidneys are working based on your age, weight, and blood creatinine level. If your estimated creatinine clearance (CrCl) drops below 50 mL/min, many drugs need a dose reduction. For example:
- Gabapentin: Standard dose is 300 mg three times a day. For CrCl <50, it’s often cut to 100-150 mg once or twice daily.
- Metformin: Stopped entirely if eGFR is below 30. Reduced dose if between 30-45.
- Amoxicillin: Standard dose may be halved in older adults with reduced kidney function.
For drugs processed by the liver, doctors look at the Child-Pugh score. This measures liver health using blood tests and physical signs. A score of 7-9 means moderate liver impairment-and a 50% dose reduction. A score of 10-15 means severe impairment. Some drugs should be avoided entirely.
Even then, it’s not just about numbers. A 72-year-old who walks slowly, gets tired easily, or forgets to eat meals might need a lower dose than a 72-year-old who hikes weekly and eats three balanced meals a day. Functional health matters as much as lab values.
The Hidden Danger: Too Many Medications
More than half of older adults take five or more prescription drugs. That’s called polypharmacy. And the more pills you take, the higher the chance of bad interactions or side effects.Anticholinergic drugs-used for overactive bladder, allergies, or depression-are especially risky. Cumulative use over time doubles the risk of dementia. Yet they’re still prescribed often. The 2023 Beers Criteria® flags 12 specific anticholinergics as high-risk.
Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen or naproxen are another trap. They’re easy to grab for joint pain. But in older adults, they raise the risk of stomach bleeding by 300% and can worsen kidney function. Acetaminophen is often safer-but even that needs limits. Too much can damage the liver, especially if you drink alcohol or take other liver-metabolized drugs.
Doctors and pharmacists now use tools like STOPP/START to review medication lists. STOPP finds potentially inappropriate prescriptions. START finds drugs that should be added but aren’t-like bone-strengthening meds for osteoporosis. But it’s not just about cutting pills. Sometimes, a lower dose of the right drug is better than stopping everything.
What You Can Do
You don’t have to wait for your doctor to bring it up. Be proactive.- Bring all your medications-prescription, over-the-counter, supplements-to every appointment. This is called a “brown bag review.”
- Ask: “Is this still necessary? Could the dose be lowered?”
- Request a medication review with a pharmacist. Many pharmacies offer this for free.
- Use a pill organizer. It helps you track what you’ve taken and when.
- Watch for side effects: dizziness, confusion, constipation, falls, nausea. Report them immediately.
Family members can help too. A 2019 study showed that when caregivers are involved, medication adherence improves by 37%. They can help spot changes in behavior or mobility that the patient might not notice.
The System Isn’t Perfect-But It’s Improving
Here’s the hard truth: most clinical trials for new drugs include very few people over 75. That means we’re often guessing how a drug will work in the oldest patients. In 2019, the FDA found that 40% of pivotal drug trials had fewer than 100 participants over 75. That’s a huge gap.But things are changing. The FDA now requires age-stratified analysis in all new drug trials. That means data must be broken down by age group. Hospitals are hiring more geriatric pharmacists. In 2015, only 41% of hospitals had one. Now, 73% do.
Technology is helping too. Electronic health records now flag when a dose is too high for kidney function. One 2020 study showed this cut dosing errors by 53%.
And AI tools are emerging. Johns Hopkins tested a program called MedAware that suggests safer doses based on age, weight, kidney function, and other meds. In a 2023 pilot, it reduced errors by 47%.
What’s Next
The future of dosing isn’t just about age. It’s about function. Doctors are starting to use simple tests-like how fast you can stand up from a chair and walk 10 feet (called the Timed Up and Go test). If it takes longer than 12 seconds, you’re likely frail. That changes how drugs are dosed.By 2030, experts predict that personalized dosing-based on real-time data from wearable sensors, lab tests, and cognitive screens-will be standard for 70% of high-risk medications. The goal? Prevent 250,000 hospitalizations a year just from bad dosing.
Right now, medication errors cost the U.S. system $1.3 trillion annually. Most of those are in older adults. The fix isn’t new drugs. It’s smarter doses. Slower starts. Better reviews. And listening to the patient-not just the chart.
Why can’t I just take the same dose as when I was younger?
Your body changes with age. Your kidneys and liver don’t clear drugs as efficiently. Your body fat increases and muscle mass decreases, which changes how drugs spread through your system. A dose that was safe at 50 can become dangerous at 75. Taking the same dose can lead to buildup in your system, causing dizziness, confusion, falls, or organ damage.
What’s the Beers Criteria® and why does it matter?
The Beers Criteria® is a list of medications that are potentially inappropriate for older adults because they carry high risks of side effects. Updated every two years by the American Geriatrics Society, it flags drugs like benzodiazepines, NSAIDs, and anticholinergics that can cause falls, dementia, or bleeding. It’s not a ban-it’s a warning. Doctors use it to avoid harmful prescriptions and choose safer alternatives.
How do I know if my dose is too high?
Watch for signs like dizziness, confusion, memory lapses, constipation, nausea, or unexplained falls. If you notice these after starting or changing a medication, talk to your doctor. Ask for a kidney function test (creatinine clearance or eGFR) and a full medication review. Don’t wait until something serious happens.
Can I stop a medication on my own if I think it’s causing problems?
No. Stopping some medications suddenly can be dangerous-like blood pressure drugs, antidepressants, or seizure meds. Even if you think it’s the culprit, talk to your doctor or pharmacist first. They can help you taper safely or switch to a better option.
Should I ask for a pharmacist to review my meds?
Yes. Pharmacists specialize in drug interactions and dosing. Many offer free medication reviews, especially for seniors on multiple prescriptions. They can spot duplications, risky combinations, and unnecessary doses. Studies show pharmacist-led reviews reduce hospitalizations by up to 22%.
What if my doctor doesn’t know about geriatric dosing?
Many primary care doctors aren’t trained in geriatric pharmacology. That’s why it’s up to you to ask. Bring the Beers Criteria® list with you. Say, “I’ve read that this drug can be risky for older adults-can we check if a lower dose or alternative is better?” If your doctor is unsure, ask for a referral to a geriatrician or clinical pharmacist.

Audrey Crothers
December 12, 2025 AT 15:16This is so important! My grandma took the same dose as me and ended up in the ER from dizziness. We didn’t know it was the meds until the pharmacist said, ‘Honey, you’re not 40 anymore.’ 😢
Reshma Sinha
December 12, 2025 AT 15:29From a clinical pharmacology standpoint, age-related changes in pharmacokinetics and pharmacodynamics necessitate individualized dosing regimens. Renal clearance declines linearly post-30, and hepatic first-pass metabolism is significantly attenuated-this isn’t anecdotal, it’s evidence-based geriatric pharmacotherapy.
Lawrence Armstrong
December 14, 2025 AT 02:19They’re not just lowering doses-they’re hiding the truth. Big Pharma doesn’t want you to know how dangerous these drugs are for seniors. They profit off the confusion. I’ve seen it. They push the same pills, then act shocked when old people fall.
Rob Purvis
December 15, 2025 AT 13:22I’ve been a geriatric nurse for 22 years, and this is still one of the most overlooked issues in primary care. I’ve had patients on 400 mg of gabapentin daily-when their CrCl was 28. They were walking like they were drunk, but the doctor said, ‘It’s just aging.’ No. It’s negligence. Start low, go slow isn’t a suggestion-it’s a lifeline. And we’re still not teaching it well in med school.
One time, a 78-year-old woman came in with confusion and falls. She was on metformin, lisinopril, and a benzo. All standard doses. We cut them all in half, then waited six weeks. Her mind cleared. She walked without a cane. That’s the power of adjusting for biology-not just defaulting to the label.
And don’t get me started on polypharmacy. It’s not just about one drug-it’s the cocktail. The Beers Criteria exists for a reason. Yet, I still see patients on 8+ meds, none of which are reviewed annually. That’s not care. That’s chaos.
Doctors need to spend more time listening, not typing. I’ve seen patients nodding along because they’re scared to say, ‘I think this is making me worse.’ We need to normalize asking: ‘Is this still helping you?’
Also, family members need to be part of the conversation. Grandkids can be the ones to say, ‘Grandma’s been tripping a lot lately-maybe check her meds?’ That’s not meddling. That’s love.
And yes, sometimes the best dose is zero. If a drug isn’t improving quality of life, it’s just adding risk. That’s hard for doctors to say. But it’s the right thing.
I wish every prescription came with a ‘For Seniors: Start Here’ sticker. It’d save so many hospital beds.
sandeep sanigarapu
December 16, 2025 AT 21:56Simple truth: bodies change. Medicine should too.
Laura Weemering
December 17, 2025 AT 20:21They say ‘start low, go slow’… but who’s really listening? I’ve watched my mother’s doctor ignore every Beers Criteria warning. She’s on five drugs she doesn’t need. And now she’s confused, tired, and falling. It’s not aging-it’s medical negligence. And nobody wants to admit it.
Why do we keep prescribing these things? Because it’s easier than talking. Because insurance won’t pay for a geriatric consult. Because the system is broken. And we’re all just… waiting for someone to die so we can say, ‘We warned you.’
It’s not just about kidneys and liver. It’s about dignity. And no one’s giving it to us.
Robert Webb
December 18, 2025 AT 15:35One thing that’s rarely discussed is how social isolation impacts medication adherence and perception of side effects. Older adults often don’t have someone to say, ‘Hey, you’ve been quieter than usual.’ Or, ‘You’re stumbling more.’ So symptoms get normalized as ‘just getting old.’
I’ve worked with dozens of seniors who’ve been on the same dose of a psychotropic for 15 years-no review, no adjustment, no conversation. The system treats them like a static data point, not a living, changing person.
And the worst part? Many don’t even know they’re on these drugs. Pills are handed out in bags with no explanation. ‘Take this once a day.’ No context. No warning. No follow-up.
It’s not just about pharmacokinetics-it’s about communication. We need to stop assuming older adults understand what they’re taking. We need to teach them, not just prescribe.
Also, caregivers need training. Not just ‘give the pill’-but ‘watch for dizziness, confusion, falls, changes in appetite.’ That’s not optional. It’s part of the treatment plan.
And yes, sometimes the best medicine is stopping something. That’s hard for doctors. But it’s the most powerful thing we can do.
Let’s stop calling it ‘geriatric medicine’ like it’s a niche. This isn’t about old people. This is about human biology. And we’re all going to get there.
Donna Anderson
December 20, 2025 AT 13:22my mom was on a benzo for sleep and she was just… gone. like, mentally. we cut it out and she came back. like, really came back. why do they even give these to old folks??
Nathan Fatal
December 22, 2025 AT 12:00This isn’t just a medical issue-it’s a philosophical one. We treat aging as a disease to be managed with pills, rather than a natural process to be respected. We optimize for longevity, not lived experience. What good is living to 90 if you’re foggy, unsteady, and on 12 drugs?
The real question isn’t ‘how do we dose better?’ It’s ‘why do we keep forcing the body to conform to a 30-year-old standard?’
Maybe the answer isn’t more science. Maybe it’s less intervention.
We’ve forgotten that sometimes, less is more. That silence, rest, and human connection can be more therapeutic than another pill.
And yet, we still reach for the prescription pad before the hand.
Levi Cooper
December 24, 2025 AT 09:10Why are we letting foreigners and bureaucrats dictate how we treat our elders? In America, we used to respect our seniors. Now we just pump them full of pills and call it care. This is what happens when you let ‘guidelines’ replace common sense.
Adam Everitt
December 24, 2025 AT 12:27start low go slow… sounds nice. but who’s actually doing it? my dad’s doc just upped his blood pressure med last month. he’s 81. he’s been dizzy since. no one checks. no one cares. just more pills.
Stacy Foster
December 25, 2025 AT 18:46They’re not adjusting doses-they’re covering up the fact that these drugs were never meant for people over 70. The FDA approved them on 20-year-olds. Now they’re giving them to grandmas and calling it ‘evidence-based.’ It’s a scam.
And don’t tell me about ‘kidney function.’ They’re not even testing it properly. They’re guessing. And our elders are paying with their balance, their minds, their lives.
Someone’s making money off this. And it’s not us.
Ashley Skipp
December 27, 2025 AT 13:26Why do doctors still give benzos to old people they know are falling? It’s not ignorance. It’s laziness. And it’s killing people