More than half of people taking medication for mental health conditions don’t take them as prescribed. It’s not laziness. It’s not weakness. It’s a complex problem rooted in how the brain works, how care is delivered, and how expensive and confusing the system can be. For someone with schizophrenia, bipolar disorder, or severe depression, missing a dose isn’t just a mistake-it can mean a return to hospitalization, a loss of housing, or worse. Yet, despite decades of awareness, adherence rates for psychiatric medications remain stuck at 40% to 60% globally. That’s not a failure of patients. It’s a failure of systems.
Why People Stop Taking Their Medication
It’s easy to assume people stop because they feel fine. But the truth is more layered. Many stop because they don’t feel like themselves. Antipsychotics can make you sluggish. Antidepressants can numb emotions. Mood stabilizers can cause weight gain or tremors. When the side effects feel worse than the illness, stopping seems like the only way to get back control. Others stop because they don’t believe they’re sick. Illness insight-knowing you have a condition that needs treatment-is often impaired in schizophrenia, bipolar disorder, and even severe depression. If you don’t think you need the medicine, you won’t take it. That’s not denial. That’s a symptom. Then there’s the cost. A single antipsychotic pill can cost $10 to $20 without insurance. Monthly, that’s hundreds. For people on fixed incomes, on Medicaid, or without coverage, choosing between meds and groceries isn’t a hypothetical. It’s daily reality. One study found homeless individuals with mental illness had adherence rates as low as 26%-not because they didn’t care, but because they couldn’t afford it. And then there’s the regimen. Taking three pills a day, at different times, with different food rules? It’s overwhelming. People forget. They get confused. They feel punished by their own treatment plan. Simpler regimens-once-daily dosing-can double adherence. Yet, in a 2024 survey, 73% of patients said their provider never even asked if simplifying their meds was an option.What Actually Improves Adherence
The good news? We know what works. And it’s not just telling people to take their pills. Pharmacist-led care is the most powerful tool we have. When pharmacists work directly with psychiatrists and patients, adherence jumps by up to 40%. These aren’t just pharmacists handing out bottles. They’re trained in mental health. They track dosing patterns. They spot side effects early. They adjust schedules. They call patients who miss appointments. In Kaiser Permanente’s Northern California program, pharmacist-led medication management led to a 32.7% increase in adherence and 18.3% fewer hospitalizations in just 90 days. Collaborative care-where a pharmacist, psychiatrist, and case manager talk regularly about each patient-cuts through the fragmentation of care. One 2025 study found patients in this model improved adherence by 1.67 points on a standard scale, nearly twice as much as those in standard care. And it saved $1,200 per patient per year in avoided hospital costs.Simplifying the Regimen
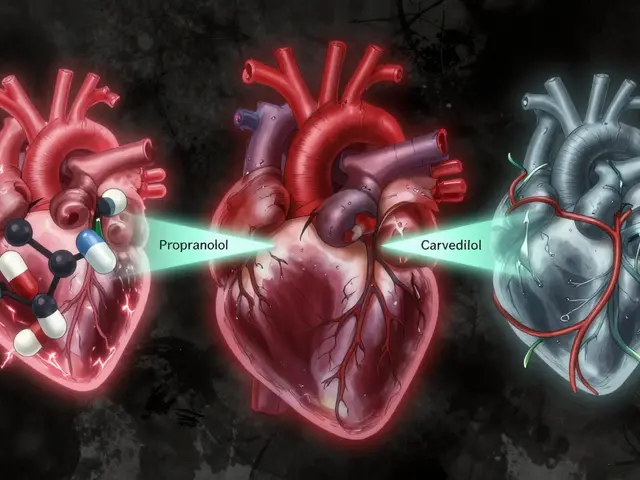
One pill a day beats three. Long-acting injectables beat daily pills. In a 2023 JAMA Psychiatry study, patients on monthly antipsychotic injections had an 87% adherence rate. Those on daily oral pills? Only 56%. That’s a 31-point gap from a single change. Yet, most providers still default to oral meds without asking if injectables are an option. Why? Tradition. Fear of patient resistance. Lack of training. But when patients are given a choice-with clear info about benefits and side effects-many choose injectables. They like not having to remember daily pills. They like fewer side effects. They like the routine of a monthly clinic visit instead of a daily ritual of doubt.
Technology Isn’t the Hero-But It Helps
Smartphone apps, pill dispensers, text reminders? They help a little. Studies show digital tools boost adherence by 1.8% to 2%. Not nothing, but not transformative. Why? Because they don’t fix the root causes: stigma, cost, side effects, or lack of human connection. But new tools are emerging. A 2025 Nature Mental Health study used smartphone sensors-how often someone opens their phone, walks, speaks-to predict when someone was likely to miss a dose. The system predicted lapses 72 hours in advance with 82.4% accuracy. That’s not surveillance. That’s early intervention. A nurse could call before the lapse happens. A pharmacist could adjust the plan. It’s proactive, not reactive.Addressing the Real Barriers
Four things make a real difference:- Predictive analytics: Systems that flag high-risk patients-those who missed three appointments, had a recent ER visit, or live in a zip code with high poverty rates-before they fall through the cracks.
- Cost transparency: Tools that show patients exactly what their meds cost, and connect them to patient assistance programs, coupons, or generics before they quit.
- Regimen simplification: Asking, “Can we reduce this to one pill a day?” or “Would a monthly shot work better?”-not assuming the original plan is the only option.
- Targeted education: Instead of saying, “Take your meds,” say, “This medicine helps stop the voices from coming back,” or “This helps you sleep so you don’t feel so hopeless.” Connect the pill to the person’s lived experience.



Ted Conerly
January 10, 2026 AT 00:54Pharmacist-led care is the quiet hero here. I’ve seen it firsthand-my cousin was cycling through ER visits until a clinical pharmacist started calling her weekly, adjusting her meds, and even driving her to appointments. Adherence jumped from 30% to 90% in four months. This isn’t theoretical. It’s life-changing. We need to fund this like we fund cancer screenings.
Faith Edwards
January 11, 2026 AT 17:24One is left to wonder, in this age of algorithmic paternalism and corporate healthcare rebranding, whether the true pathology lies not in the patient’s noncompliance, but in the grotesque epistemological arrogance of a system that presumes to know what ‘adherence’ means without ever having sat across from someone who has lost their sense of self to a pill bottle. The tragedy is not that they forget-they are forgotten.
Jay Amparo
January 13, 2026 AT 11:03In India, we have this saying: ‘Dawa nahi, dard ka ilaj chahiye.’ Medicine isn’t the cure-the pain needs to be understood. I’ve seen people skip antipsychotics because the side effects made them feel like ghosts. But when a community health worker sat with them for an hour every week-not to remind, but to listen-adherence improved. It’s not about pills. It’s about presence.
Lisa Cozad
January 14, 2026 AT 16:02My sister has bipolar disorder. She tried six different meds over five years. The one that stuck? A once-daily mood stabilizer with a simple text reminder. No fancy app. Just a text from her sister at 8 a.m. every day. Sometimes the simplest things are the most powerful. We don’t need tech breakthroughs-we need someone who cares enough to show up.
Saumya Roy Chaudhuri
January 15, 2026 AT 07:48Let’s be real-most people don’t take their meds because they’re lazy, delusional, or just don’t care. The system doesn’t fail them; they fail themselves. If you can’t manage to take a pill once a day, maybe you’re not ready for independence. Stop romanticizing noncompliance. It’s not a social justice issue-it’s personal responsibility.
anthony martinez
January 16, 2026 AT 13:12So let me get this straight-we’re going to spend millions on predictive analytics to tell us who’s going to skip their meds… but we won’t pay for the meds themselves? Brilliant. Next up: AI that predicts which patients will forget to breathe and sends them a reminder. Maybe we should just start charging people rent for having a brain.
lisa Bajram
January 17, 2026 AT 19:59OH MY GOD-THIS IS SO IMPORTANT!! I’ve been screaming this from the rooftops!! Long-acting injectables? YES!! My cousin was terrified of needles, but after one shot, she said, ‘I feel like I can finally breathe again.’ No daily panic. No guilt. Just stability. Why isn’t this the default?! We need to stop treating mental health like it’s optional!!
Michael Marchio
January 19, 2026 AT 01:21It’s fascinating how the narrative has shifted from ‘patients are noncompliant’ to ‘the system is broken’-a classic case of institutional self-absolution. While systemic failures are undeniable, one must not ignore the fundamental human tendency toward avoidance, particularly when the discomfort of treatment exceeds the abstract dread of potential relapse. The notion that simplification alone will resolve adherence is dangerously reductive; the human psyche is not a software bug to be patched with a once-daily dose.
Jake Kelly
January 20, 2026 AT 14:23I work in a community clinic. We tried adding a pharmacist. Lasted six months. Budget got cut. Staff were overwhelmed. No one had time to train. We all agreed it was the right thing. But ‘right’ doesn’t pay the bills. The system isn’t broken-it’s rigged. And until we fix the funding, all the ‘what works’ studies are just pretty words on a page.
Jaqueline santos bau
January 20, 2026 AT 20:11Ugh, I can’t believe people still think this is just about ‘taking pills.’ My cousin was hospitalized TWICE because she couldn’t afford her meds-and now she’s living in her car. And the worst part? The nurses at the ER kept saying, ‘Why didn’t you just take your medicine?’ Like it was her fault. Like she didn’t cry herself to sleep every night wondering if she’d ever feel normal again. This isn’t about compliance. It’s about survival.
chandra tan
January 22, 2026 AT 01:07In my village, we don’t have pharmacies. We have neighbors. When someone skips their meds, someone else brings them a cup of tea and says, ‘You good today?’ No apps. No texts. Just presence. Maybe the answer isn’t tech-it’s community.
Dwayne Dickson
January 22, 2026 AT 10:08While the structural imperatives outlined are indeed laudable, one must interrogate the ontological assumption underpinning this discourse: that adherence is a measurable, quantifiable outcome amenable to interventionist protocols. The very notion of ‘adherence’ presumes a Cartesian dichotomy between patient and pathogen-a reductionist framework that pathologizes subjective experience as noncompliance. The pharmacological paradigm, while efficacious in some cases, fails to account for the phenomenological rupture that accompanies psychiatric illness. One cannot optimize a life through dosage schedules alone.
Mario Bros
January 23, 2026 AT 09:45My uncle took his meds for 10 years. Then stopped. Said he felt ‘numb.’ We didn’t push. We just asked, ‘What do you miss?’ He said, ‘Laughing.’ So we started taking him to open mic nights. He got a hobby. He started sleeping better. He’s back on meds now-because he wanted to, not because he was told to. Sometimes, healing isn’t in the pill. It’s in the joy.
Jake Nunez
January 24, 2026 AT 06:51Long-acting injectables are the future. My therapist pushed me to try one. I was scared. Now I get a shot once a month. No daily guilt. No wondering if I took it. I sleep better. I work full-time. It’s not magic. It’s just… simpler. Why don’t more doctors offer this like they offer insulin for diabetics?
Paul Bear
January 25, 2026 AT 17:56It is statistically and empirically demonstrable that non-adherence correlates strongly with socioeconomic deprivation, cognitive impairment, and lack of social support-not with ‘systemic failure.’ The conflation of structural inequity with individual agency is not only logically flawed, it is ethically dangerous. If we remove personal accountability from the equation, we abdicate the moral responsibility of the patient to reclaim agency over their own recovery. This is not compassion-it is infantilization.