Levodopa: What It Is, How It Works, and What You Need to Know
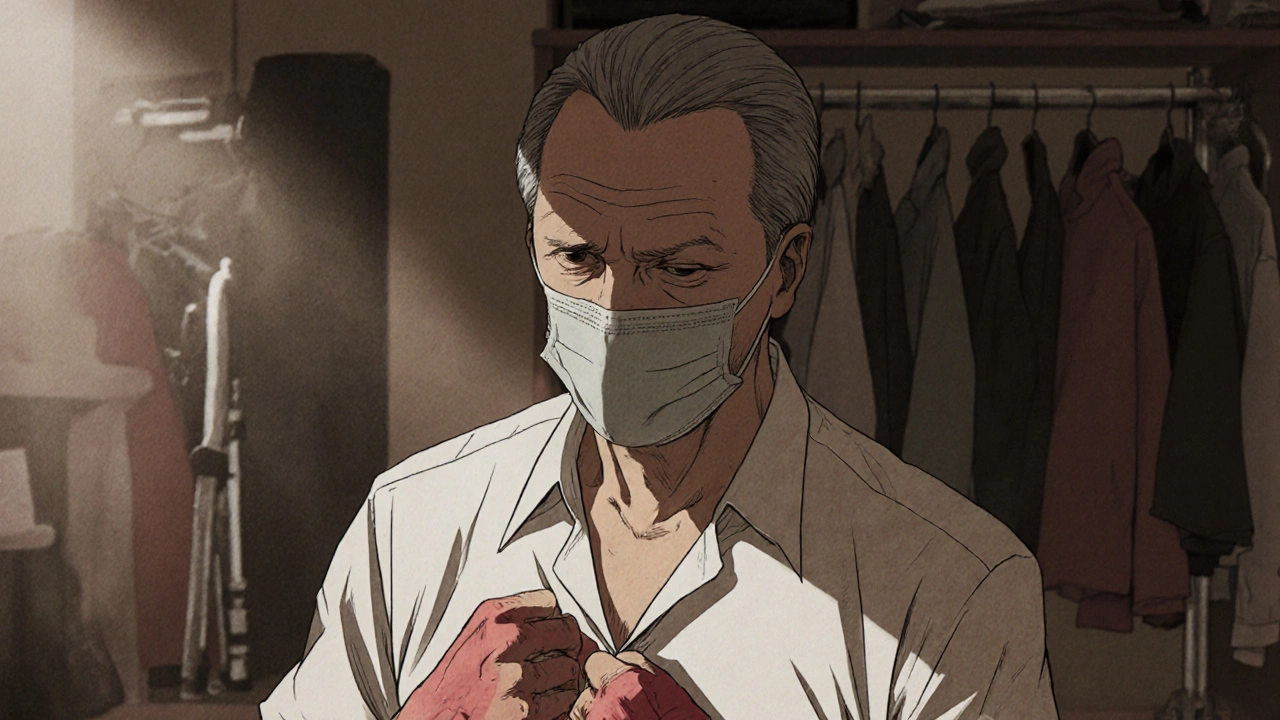
When your brain stops making enough levodopa, a chemical that the body converts into dopamine to help control movement. Also known as L-DOPA, it's the gold standard treatment for Parkinson’s disease. Without enough dopamine, movements become slow, stiff, or shaky—symptoms that make everyday tasks like buttoning a shirt or walking across a room feel impossible. Levodopa doesn’t cure Parkinson’s, but for millions, it’s the difference between being stuck and being able to move.
Levodopa rarely works alone. It’s almost always paired with carbidopa, a drug that stops levodopa from breaking down before it reaches the brain. Without carbidopa, most of the levodopa gets used up in the body before it can help the brain, leading to nausea, low blood pressure, and wasted doses. Together, they let you take less levodopa and get better results. This combo is what you’ll find in popular brands like Sinemet and Rytary. It’s not fancy, but it’s proven—used safely for over 50 years.
Levodopa doesn’t work the same for everyone. Some people get great relief for years. Others notice their symptoms return faster between doses, or they start having sudden, unpredictable shifts between moving well and freezing up. These are called "on-off" fluctuations, and they often show up after 5–10 years of use. That’s why doctors watch closely—adjusting doses, timing, or adding other meds like dopamine agonists, drugs that mimic dopamine’s effect in the brain. Some patients also need to avoid high-protein meals around dosing time, since protein can block levodopa from being absorbed.
It’s not all smooth sailing. Long-term use can lead to involuntary movements called dyskinesias—jerky or twisting motions that can be as troubling as the original symptoms. That’s why doctors start with the lowest effective dose and avoid pushing higher too fast. Still, for most people with Parkinson’s, the benefits far outweigh the risks. No other single drug comes close to restoring movement the way levodopa does.
What you won’t find in a pill bottle is the full picture: how levodopa interacts with sleep, mood, and even digestion. Some users report sudden sleep attacks, sudden drops in blood pressure, or hallucinations—especially in older adults. That’s why monitoring isn’t optional. It’s part of the treatment. And while newer treatments like deep brain stimulation or continuous infusion pumps exist, levodopa remains the foundation. It’s the first line, the most studied, and still the most trusted.
Below, you’ll find real-world guides on how levodopa fits into broader treatment plans, how it compares to other Parkinson’s drugs, and what to watch for when taking it long-term. These aren’t theory pieces—they’re practical, tested insights from people who’ve lived with the medication and doctors who’ve managed its use for decades. Whether you’re newly diagnosed or have been on it for years, there’s something here that can help you take better control.