Pancreatic Duct Blockage: What It Looks Like and How It's Treated
A blocked pancreatic duct can cause sudden, severe belly pain and lead to pancreatitis. If you feel intense upper abdominal pain that radiates to your back, get medical help quickly. This page explains why ducts block, how doctors find the problem, and what treatments usually work—so you know what to expect.
Diagnosis and tests
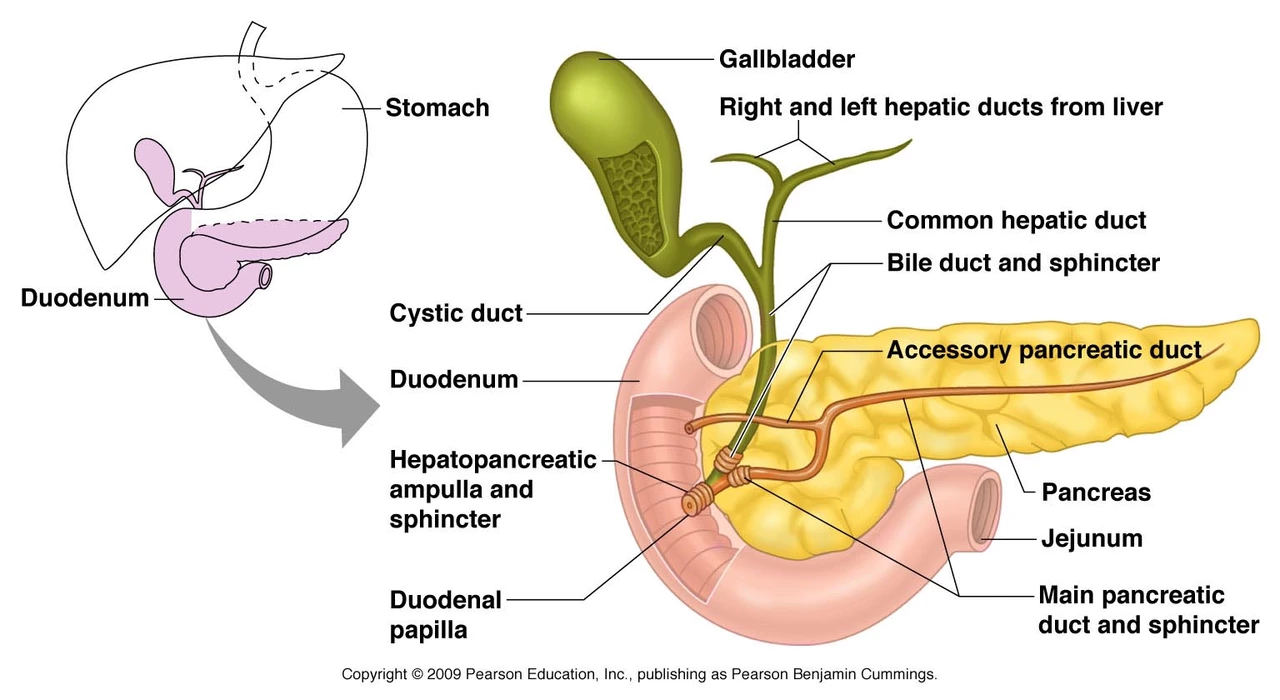
Doctors start with a quick history and blood tests. High amylase or lipase suggests pancreatitis. Liver blood tests can point to a bile duct or pancreatic head problem. Imaging is next: abdominal ultrasound often spots gallstones. CT scan shows inflammation, complications, and fluid collections. MRCP (MRI for the bile and pancreatic ducts) is noninvasive and useful for spotting strictures or stones inside the duct. ERCP combines a camera and X-ray and can both find and fix blockages, but it carries a small risk of causing pancreatitis. Endoscopic ultrasound (EUS) can detect small tumors or stones that other scans miss.
Treatment and home care
Treatment depends on the cause. If gallstones are stuck, doctors often remove them with ERCP and may follow with gallbladder surgery later. Strictures (narrowing) from chronic pancreatitis can get temporary or permanent stents placed by endoscopy. Tumors require surgery, oncology referral, or stenting to relieve obstruction. Infected collections or pseudocysts may need drainage. For pain and acute attacks you’ll get IV fluids, pain control, and sometimes antibiotics if infection is suspected.
Long-term care focuses on protecting digestion and preventing malnutrition. If the pancreas makes fewer enzymes, your doctor may prescribe pancreatic enzyme replacement (pancrelipase) to help digest fats and proteins. You may need to limit dietary fat, take fat-soluble vitamins (A, D, E, K) if levels fall, stop alcohol completely, and quit smoking—both make pancreatic problems worse.
At home, rest, small frequent meals, and following the low-fat plan your care team gives are useful. Keep track of stools—fatty or oily stool (steatorrhea) suggests enzyme need. If you’re on enzyme pills, take them with meals for best effect.
Know the red flags: worsening or unrelieved pain, persistent vomiting, fever, yellowing skin or eyes, or fainting require urgent care. Ask your provider: what caused my blockage, do I need ERCP or surgery, should I start enzyme treatment, and what follow-up imaging is needed?
Blocked pancreatic ducts can be scary, but many causes are treatable. Quick diagnosis and the right procedure—often ERCP or stenting—reduce complications. Stick to follow-up, avoid alcohol and tobacco, and get help fast if symptoms worsen.