Introduction to Tacrolimus
Tacrolimus, also known as FK506, is a widely used immunosuppressive drug. It has become a vital part of organ transplant medicine and is also used to treat certain autoimmune diseases. As a blogger with a keen interest in science and medicine, I am excited to delve deep into the science behind Tacrolimus and explore its mechanism of action. In this article, we will discuss the various aspects of this fascinating drug, including its discovery, chemical structure, pharmacokinetics, and clinical applications. So, let's embark on a journey to learn more about this life-saving medication.
The Discovery of Tacrolimus
The story of Tacrolimus begins in the 1980s with the search for new immunosuppressive agents to improve the outcomes of organ transplantation. Researchers were looking for substances that could prevent the body's immune system from attacking transplanted organs, thereby reducing the risk of rejection. It was during this search that a team of scientists from Fujisawa Pharmaceutical Company (now Astellas Pharma) in Japan discovered a unique compound produced by a soil bacterium called Streptomyces tsukubaensis. This compound was named Tacrolimus, and its remarkable immunosuppressive properties quickly caught the attention of the scientific community.
Chemical Structure and Properties of Tacrolimus
Tacrolimus is a macrolide, a type of large, complex molecule with a characteristic macrocyclic lactone ring structure. This ring structure is essential for the immunosuppressive properties of Tacrolimus. The molecule also contains several additional functional groups, which contribute to its lipophilicity and high binding affinity to its target proteins. These properties make Tacrolimus a highly potent and specific immunosuppressive agent, allowing it to effectively modulate the immune system's response to transplanted organs and other foreign substances.
Pharmacokinetics: How Tacrolimus Works in the Body
Understanding the pharmacokinetics of Tacrolimus is crucial to appreciate how this drug works in the body. Tacrolimus is usually administered orally or intravenously, and its absorption varies depending on the route of administration and individual factors such as the patient's age, weight, and genetics. Once absorbed into the bloodstream, Tacrolimus binds to a specific intracellular protein called FK506-binding protein (FKBP). This protein-drug complex then interacts with another protein called calcineurin, inhibiting its activity. Calcineurin is a critical enzyme in the activation of T-cells, a type of white blood cell responsible for the immune response. By inhibiting calcineurin, Tacrolimus effectively suppresses the immune system, preventing it from attacking transplanted organs and causing rejection.
Immunosuppressive Effects of Tacrolimus
The primary mechanism by which Tacrolimus exerts its immunosuppressive effects is through the inhibition of calcineurin, as mentioned earlier. This inhibition prevents the activation of T-cells, which play a crucial role in the immune response. By suppressing T-cell activation, Tacrolimus effectively dampens the body's immune response to foreign antigens, such as those found on transplanted organs. In addition to its effects on T-cells, Tacrolimus has also been shown to modulate the function of other immune cells, such as B-cells and macrophages, further contributing to its overall immunosuppressive properties.
Tacrolimus in Organ Transplantation
Since its discovery, Tacrolimus has become a cornerstone of immunosuppressive therapy in organ transplantation. It is used in combination with other immunosuppressive drugs, such as corticosteroids and mycophenolate mofetil, to prevent acute and chronic rejection of transplanted organs, including kidneys, livers, hearts, and lungs. The use of Tacrolimus has significantly improved the outcomes of organ transplantation, allowing patients to lead healthier and more extended lives after their surgeries. However, like any medication, Tacrolimus has its risks and side effects, which must be carefully monitored and managed by healthcare professionals.
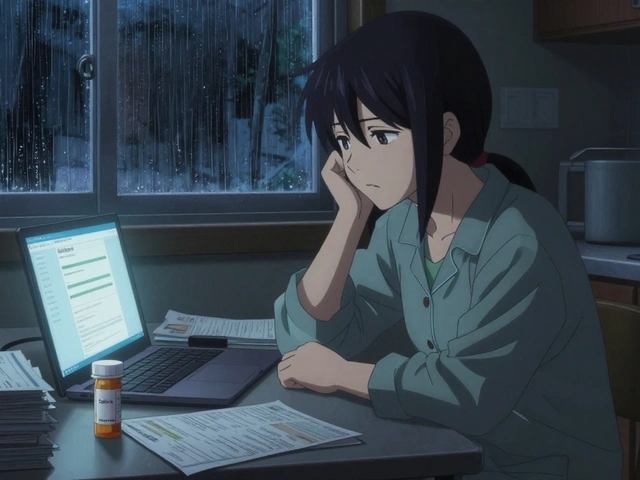
Side Effects and Risks of Tacrolimus
While Tacrolimus is a highly effective immunosuppressive agent, its use is not without risks. Some of the common side effects associated with Tacrolimus include hypertension, hyperglycemia, nephrotoxicity, neurotoxicity, gastrointestinal disturbances, and an increased risk of infections. Additionally, long-term use of Tacrolimus has been linked to an increased risk of certain malignancies, such as lymphomas and skin cancers. To minimize these risks, patients on Tacrolimus therapy must be closely monitored, and their dosages carefully adjusted to balance the benefits of immunosuppression against the potential side effects.
Tacrolimus in Autoimmune Diseases
Aside from its use in organ transplantation, Tacrolimus has also been studied for its potential applications in treating autoimmune diseases. Autoimmune diseases occur when the body's immune system mistakenly attacks its own tissues, causing inflammation and tissue damage. Given its immunosuppressive properties, Tacrolimus has shown promise in treating certain autoimmune diseases, such as atopic dermatitis, rheumatoid arthritis, and lupus nephritis. However, more research is needed to fully understand the role of Tacrolimus in the management of these conditions and to establish its long-term safety and efficacy.
Conclusion: The Future of Tacrolimus
In conclusion, Tacrolimus is a remarkable drug that has revolutionized the field of organ transplantation and holds promise for the treatment of autoimmune diseases. Its unique mechanism of action offers a highly effective means of modulating the immune system, providing life-saving benefits to countless patients around the world. As our understanding of the science behind Tacrolimus continues to evolve, we can look forward to new developments and innovations in the use of this powerful immunosuppressive agent. The future of Tacrolimus is undoubtedly bright, and I am excited to see what new discoveries lie ahead.



richard king
May 8, 2023 AT 21:18Delving into the alchemy of Tacrolimus feels like wandering through a secret garden of molecular intrigue, where each ring of its macrolide skeleton whispers promises of grafted harmony. The journey from a humble soil bacterium to a lifesaving pharmacological marvel underscores the audacity of scientific curiosity. It is a testament to humanity’s relentless pursuit of solutions that dance on the edge of chemistry and biology. In reading this exposition, one cannot help but feel a swell of reverence for the silent battles waged within our cells.
Dalton Hackett
May 8, 2023 AT 22:00Reading through the detailed breakdown of Tacrolimus, I was immediately struck by the intricate interplay of structural chemistry and immunological pathways, which the author has articulated with commendable thoroughness. The description of the macrolide's macrocyclic lactone ring not only highlights its significance in binding affinity but also serves as a reminder of the delicate balance required to achieve therapeutic potency without undue toxicity. Moreover, the pharmacokinetic nuances, such as variations in oral versus intravenous absorption, bring to light the personalized considerations clinicians must navigate. The binding of Tacrolimus to FKBP, followed by the inhibition of calcineurin, is elegantly summarized, yet the cascading downstream effects on T‑cell activation could benefit from a deeper exploration of transcription factor modulation. It is also noteworthy that the article acknowledges the drug’s impact beyond transplantation, touching upon autoimmune applications, which opens a broader clinical horizon. The side‑effect profile, while comprehensive, might have underscored the prevalence of nephrotoxicity in a more quantified manner, perhaps referencing recent meta‑analyses. Additionally, a brief comparison with cyclosporine could have contextualized Tacrolimus’s relative advantages. The historical anecdote regarding its discovery in the 1980s provides a pleasant narrative backdrop, linking scientific serendipity to modern therapeutic breakthroughs. Overall, the piece serves as a solid foundation for both novices and seasoned professionals seeking to understand this cornerstone immunosuppressant, though certain areas beckon for expanded discourse to fully capture the drug’s multifaceted character.
William Lawrence
May 8, 2023 AT 22:50Oh great, another drug that “revolutionized” everything, as if we needed more hype.
Grace Shaw
May 8, 2023 AT 23:40I would like to express my sincere appreciation for the comprehensive nature of this article. The author has demonstrated an admirable command of the subject matter, particularly in elucidating the pharmacodynamic mechanisms underlying Tacrolimus therapy. It is evident that considerable scholarly effort has been invested in compiling the historical context, structural chemistry, and clinical implications. Such rigor not only informs but also enhances the discourse within the medical community. I respectfully encourage the inclusion of recent clinical trial data to further substantiate the therapeutic outcomes discussed herein.
Sean Powell
May 9, 2023 AT 00:30yeah totally agree with Grace this stuff is like a cultural bridge between chemists and docs we all learn from each othr and it’s cool how tacrolimus connects the dots without being all stiff and formal
Henry Clay
May 9, 2023 AT 01:20Honestly the risks are way underplayed here : high blood pressure, kidney damage – not a joke 😊 doctors need to be real about dosing.
Isha Khullar
May 9, 2023 AT 02:10The poetic dance of immunosuppression meets the cold harshness of side effects it is a tragic beauty that reminds us of our fragile mortality