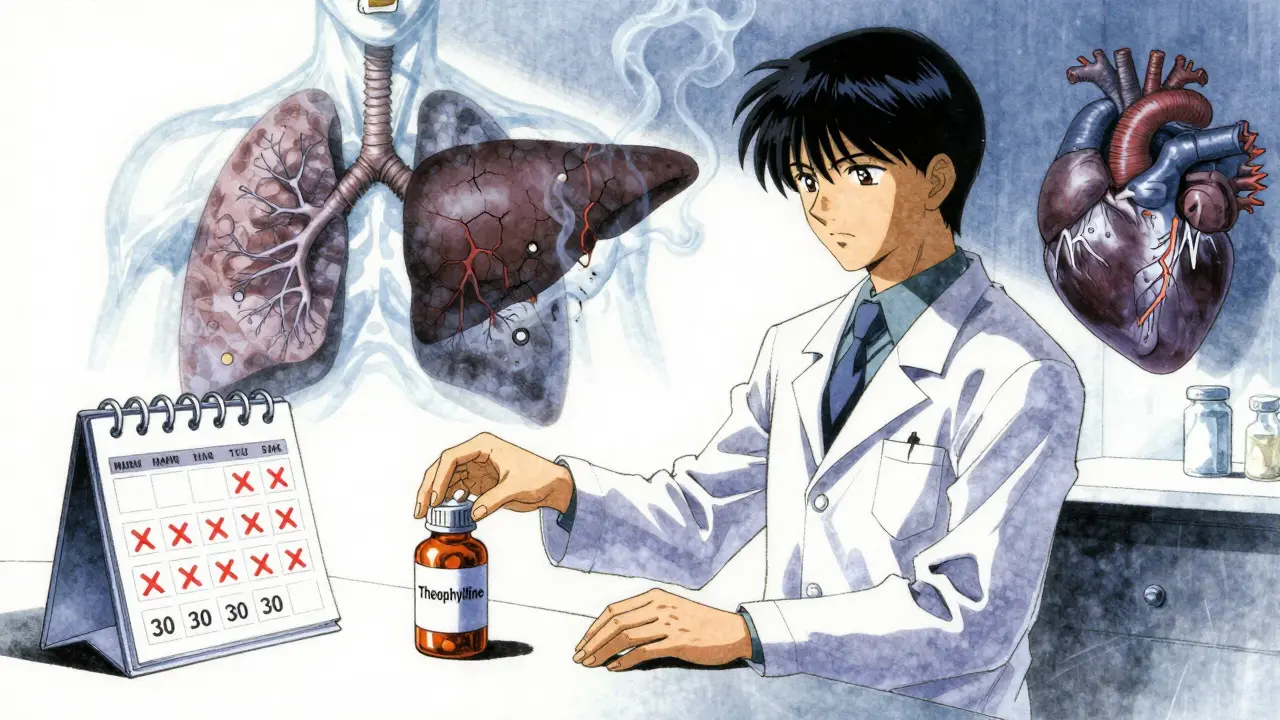
When a drug has a narrow therapeutic index, even a tiny mistake in dosing can turn treatment into danger. Theophylline is one of those drugs. Used for decades to treat asthma and COPD, it’s cheap, effective, and still in use today - but only if you monitor it closely. Without regular blood tests, the line between healing and hospitalization is razor-thin.
What Makes Theophylline So Risky?
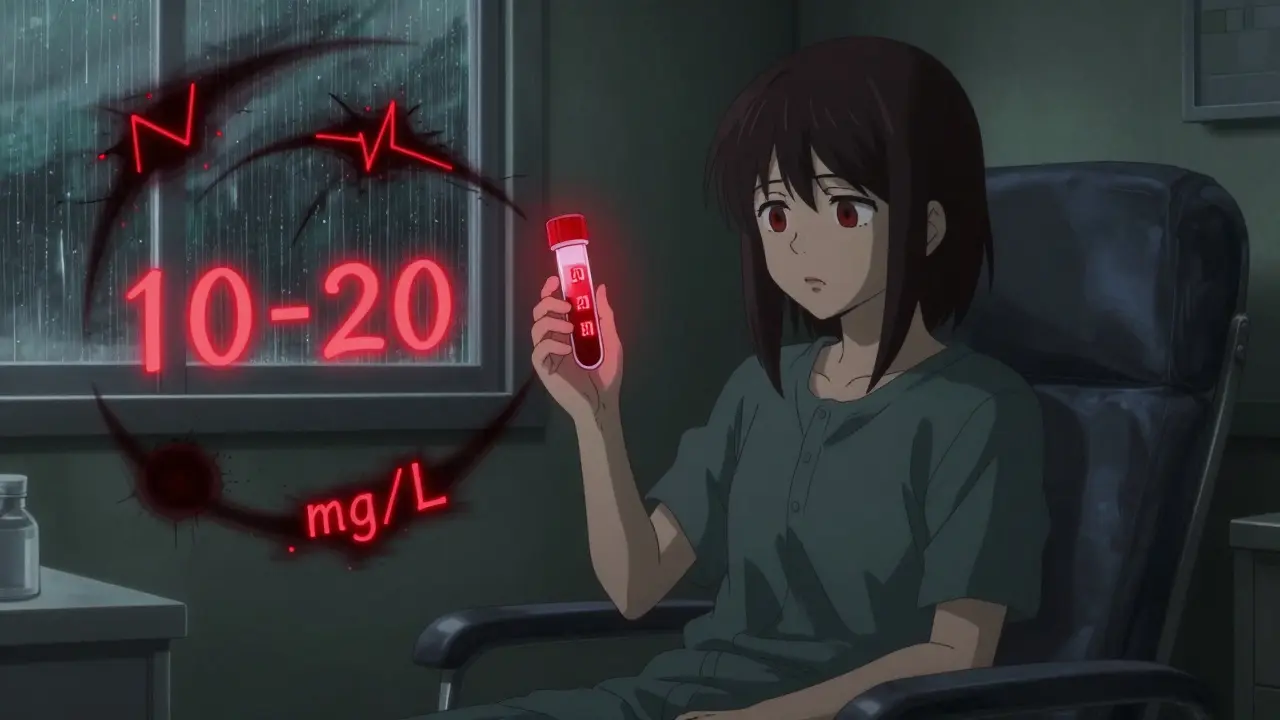
Theophylline works by relaxing the airways and reducing lung inflammation. It’s not a first-line treatment anymore - inhaled steroids and long-acting bronchodilators are preferred. But for some patients with severe, uncontrolled asthma or COPD, theophylline still makes a difference. The problem? Its safe range is incredibly small: 10 to 20 mg/L. Go below 10, and it barely helps. Go above 20, and you risk seizures, irregular heartbeats, vomiting, or worse.
At 25 mg/L or higher, the risk of death climbs sharply. In the U.S., about 1,500 people end up in emergency rooms each year because of theophylline toxicity. Around 10% of those cases are fatal. That’s not a small risk. It’s a warning sign that this drug demands respect.
Why Can’t You Just Guess the Right Dose?
You might think, ‘I’ll start with 200 mg a day and see how I feel.’ That’s a dangerous assumption. Theophylline doesn’t behave like most drugs. Its metabolism is unpredictable and changes based on things you can’t control.
Smokers clear the drug 50-70% faster than non-smokers. That means a smoker might need twice the dose of a non-smoker just to reach the same blood level. Stop smoking, and suddenly that same dose becomes toxic. Alcohol? It can lower levels. Pregnancy? Levels drop by 30-50% in the third trimester. Liver disease? Clearance can drop by more than half. Heart failure? Same thing.
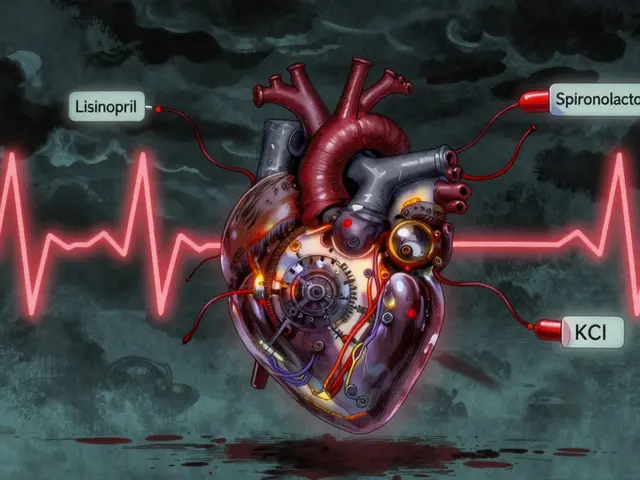
And then there are the drug interactions. Take clarithromycin or ciprofloxacin? Your theophylline levels can spike by 65% in just a few days. That’s what happened to a 68-year-old man in a 2023 case report - he developed life-threatening heart rhythm problems after starting an antibiotic. He wasn’t told to get his levels checked. He didn’t know to ask. He ended up in intensive care.
When and How Often Should You Test?
Testing isn’t optional. It’s part of the treatment. The first test should happen 5 days after starting theophylline - or 3 days after any dose change. That’s how long it takes for the drug to reach a steady level in your blood.
For immediate-release tablets, blood is drawn right before your next dose - that’s the trough level. For extended-release versions, it’s done 4 to 6 hours after taking the pill. Getting it wrong means you’re not measuring what you think you are.
Once you’re stable, you still need checks every 6 to 12 months. But if you’re over 60, have heart or liver problems, or are pregnant, you need them every 1 to 3 months. Monthly during pregnancy. That’s not overkill - it’s necessary. Your body changes. The drug’s effect changes with it.
And if you start a new medication, stop smoking, get sick, or drink more alcohol than usual - test again. No exceptions.
It’s Not Just About the Number
A blood test tells you the level, but it doesn’t tell you the whole story. You also need to watch for signs of toxicity: nausea, tremors, rapid heartbeat, trouble sleeping, or confusion. These aren’t just side effects - they’re red flags.
Doctors should also check your potassium. Theophylline is often used with other drugs like albuterol or steroids, which can drain potassium. Low potassium makes heart rhythm problems more likely. A full blood count helps catch rare bone marrow issues. And if you’re getting the drug through an IV, the infusion site needs checking - mixing it with dextrose can cause dangerous clumping or cell damage.
One patient in a 2022 study went from poorly controlled asthma to near-normal breathing after a simple protocol was introduced: blood tests every 3 months, dose adjustments based on results, and education for both patients and staff. Adverse events dropped by 78%. Asthma control improved by 35%. That’s not magic. That’s monitoring.
Why Do Some Doctors Still Skip It?
A 2024 study suggested low-dose theophylline (200 mg/day) might be safe without monitoring. But that’s not the consensus. The European Respiratory Society, the American Thoracic Society, and the NHS all say: no monitoring, no theophylline. Period.
Why? Because even at low doses, metabolism varies wildly. One patient might take 200 mg and stay at 8 mg/L. Another might hit 22 mg/L on the same dose. There’s no way to predict who will react how. That’s why blanket rules don’t work. Individual monitoring does.
And here’s the truth: many patients aren’t warned. They’re handed a script and told to take it. No one explains the risks. No one schedules the blood test. By the time symptoms show up, it’s too late.

The Bigger Picture: Cost vs. Risk
Theophylline costs $15 to $30 a month. New biologic treatments for asthma can cost $200 to $400 a month. That’s why it’s still used - especially in places with limited resources. But saving money on the drug shouldn’t mean risking your life.
Every year, poison control centers see a 23% increase in theophylline toxicity cases. Most involve older adults with undiagnosed liver or kidney problems. These aren’t overdoses. These are failures of monitoring.
There’s hope on the horizon. Companies are testing handheld devices that could give you a theophylline reading in under five minutes - like a glucose meter. But until those are widely available and proven, the only safe way is the old way: a blood draw, a lab, and a doctor who knows what to do with the result.
What You Should Do
- If you’re prescribed theophylline, ask: ‘When is my next blood test?’
- Keep a log of all other medications, supplements, and changes in smoking or drinking habits.
- Don’t skip tests just because you feel fine. Toxicity doesn’t always come with obvious symptoms.
- Know the warning signs: nausea, rapid heartbeat, shaking, confusion. Call your doctor immediately if they appear.
- Ask for a copy of your results. Understand your target range: 10-20 mg/L. Anything outside that needs action.
Theophylline isn’t a drug you take and forget. It’s a tool that needs constant tuning. Like a car with a sensitive engine, it runs perfectly - until it doesn’t. And when it fails, it fails hard.
Monitoring isn’t an inconvenience. It’s the difference between breathing easier and fighting for your life.

Skye Kooyman
January 27, 2026 AT 01:50Just took my theophylline this morning. Felt fine. Didn't think twice. Now I'm reading this and wondering if I'm one tick away from the ER.
Shawn Raja
January 28, 2026 AT 08:33Oh wow. So we're still using a drug from the 1950s that could kill you if your coffee intake goes up? Brilliant. The pharmaceutical industry doesn't invent new drugs-they just repackaging death traps with a side of 'trust us, bro.'
And yet somehow, the $400/month biologics get all the press while this $20 relic sits in the corner like a ticking bomb with a prescription label. We're not saving money-we're gambling with people's lives and calling it 'cost-effective.'
Also, why does no one tell patients this? You get a script, you go home, you take it. No warning. No blood test schedule. No 'hey, if you start smoking again, you might die.' Just silence. That's not healthcare. That's negligence with a stethoscope.
Ryan W
January 29, 2026 AT 20:14It's not that complicated. If you're prescribing theophylline, you're responsible for monitoring. End of story. The fact that some clinicians are skipping labs is a systemic failure, not a pharmacological one.
Therapeutic drug monitoring isn't optional-it's standard of care. The FDA, EMA, and ATS all mandate it. If your facility isn't doing it, you're practicing below the standard. Period. No excuses. No 'but my patient felt fine.' Feeling fine doesn't mean the serum level isn't at 27 mg/L.
Allie Lehto
January 31, 2026 AT 19:16OMG I JUST REALIZED MY DAD TOOK THIS FOR YEARS AND NEVER GOT TESTED 😭
He's 72, has COPD, smokes (still!!), and takes cipro every time he gets a sinus infection. I just cried reading this. How many people are just... living on a knife's edge and don't even know it?
Also why is no one talking about how the system fails the elderly? They're handed pills like candy and told 'take one a day.' No one checks if they're even swallowing them right. This is a tragedy waiting to happen in every nursing home in America.
TONY ADAMS
February 2, 2026 AT 16:13bro i took this once and felt like my heart was gonna explode. i thought it was anxiety. turns out i was at 24 mg/L. i didn't even know what theophylline was. just took it because the doc said so.
now i just use my inhaler and chill. why do they even make this stuff?
Napoleon Huere
February 3, 2026 AT 14:33This is the kind of post that makes you realize medicine isn't magic-it's math. And bad math kills.
Theophylline isn't a drug you take. It's a variable you manage. Like a reactor core. You don't just turn it on and walk away. You monitor the neutron flux. You adjust the control rods. You watch the temperature.
And yet we treat it like aspirin. We hand it out like candy and expect the body to behave predictably. But the body doesn't care about our protocols. It adapts. It changes. It breaks.
So why are we still surprised when it fails?
Shweta Deshpande
February 5, 2026 AT 10:07I'm from India and we use theophylline ALL THE TIME here because it's cheap and accessible. I've seen so many patients on it-grandmas, uncles, neighbors-and not one of them ever got blood tests. They just take it and hope.
But I'm so glad someone wrote this. Maybe now, when my cousin starts on it, I can show her this and say, 'No, you need to get tested. Even if you feel fine.'
It's not about fear. It's about care. And care doesn't have to be expensive. It just has to be consistent.
Thank you for writing this. I'm sharing it with my whole family.
Aishah Bango
February 7, 2026 AT 05:49People who don't monitor theophylline are playing Russian roulette with their organs. There's no excuse. Not 'I forgot.' Not 'I felt okay.' Not 'It's too expensive.'
If you're okay with risking seizures, arrhythmias, or death because you're too lazy to schedule a blood test-you're not just irresponsible. You're dangerous.
And if your doctor lets you skip it? Fire them.
Simran Kaur
February 9, 2026 AT 05:19I just read this and I'm crying. Not because I'm scared-I'm crying because I finally understand why my aunt kept saying she felt 'off' after her meds changed. She didn't know it was the theophylline. No one told her. She thought it was just aging.
Now I'm going to call her and make sure she gets tested next week. And I'm going to ask my own doctor if I ever need this-because I don't want to be one of those people who almost dies because no one bothered to check.
Thank you for giving us the words to say, 'Wait, this isn't normal.'
Neil Thorogood
February 9, 2026 AT 12:15THEOPHYLLINE: the drug that makes your heart race, your hands shake, and your doctor look guilty when you ask, 'Why didn't you test me?' 🤡
Look, I get it. It's cheap. It works. But if your treatment plan includes 'hope for the best,' you're not a patient-you're a beta tester.
Get your blood drawn. Keep a log. Tell your doc when you drink coffee. Don't be the guy who dies because he thought 'it's just a pill.'
Also, if you're on this and you smoke? Stop. Or at least tell someone before you keel over. Your liver isn't a superhero.
Jessica Knuteson
February 10, 2026 AT 09:23Monitoring is mandatory. But the fact that it's not universally done proves the system is broken. Not the drug. Not the patients. The system.
Cost savings ≠ safety. And pretending otherwise is dangerous.
James Nicoll
February 11, 2026 AT 07:01It's funny how we treat theophylline like it's some ancient relic from the dark ages. But it's not the drug that's outdated-it's our attitude toward it.
We've become so obsessed with 'newer, better, pricier' that we forget the simple stuff. Blood tests. Patient education. Consistency.
Maybe the real innovation isn't a new biologic. Maybe it's just remembering to check the numbers before you assume everything's fine.
Uche Okoro
February 12, 2026 AT 07:43In Nigeria, we use theophylline because we have no choice. We don't have the labs, the infrastructure, or the staff to monitor every patient. So we give it anyway. We pray.
This post is accurate. But it's also a luxury. In places where you have to choose between antibiotics and blood tests, 'monitoring' is a fantasy.
Don't judge. Advocate. Push for access. Don't just say 'you should get tested.' Say 'how can we make testing possible?'
Peter Sharplin
February 13, 2026 AT 19:02I'm a respiratory therapist. I've seen this too many times. A patient comes in with palpitations, tremors, nausea. We check the theophylline level. 28 mg/L. They were on 200 mg/day. Non-smoker. No new meds.
Turns out they started drinking grapefruit juice every morning. Didn't think it mattered.
It matters. A lot.
Every single time I see this, I make sure the patient leaves with a printed sheet: 'Things That Change Your Theophylline Level.' And I make them read it out loud. Because if they don't understand it, they won't remember it.
It's not complicated. It's just not taught well.
John Wippler
February 15, 2026 AT 01:26Imagine a car that runs perfectly… until it doesn't. Then it explodes.
That's theophylline. You don't need a fancy dashboard to drive it-you need a mechanic who checks the oil every 500 miles.
Most doctors treat it like a Prius. But it's a turbocharged race car with no gauges.
And yet, we keep handing out keys to people who've never taken driver's ed.
It's not the drug's fault. It's ours. We stopped teaching the basics.
Let's fix that. Not with more drugs. With more vigilance.