Smoking & Alcohol Impact on Acid Indigestion
Your Personalized Risk Analysis
Key Factors Identified:
Recommended Actions:
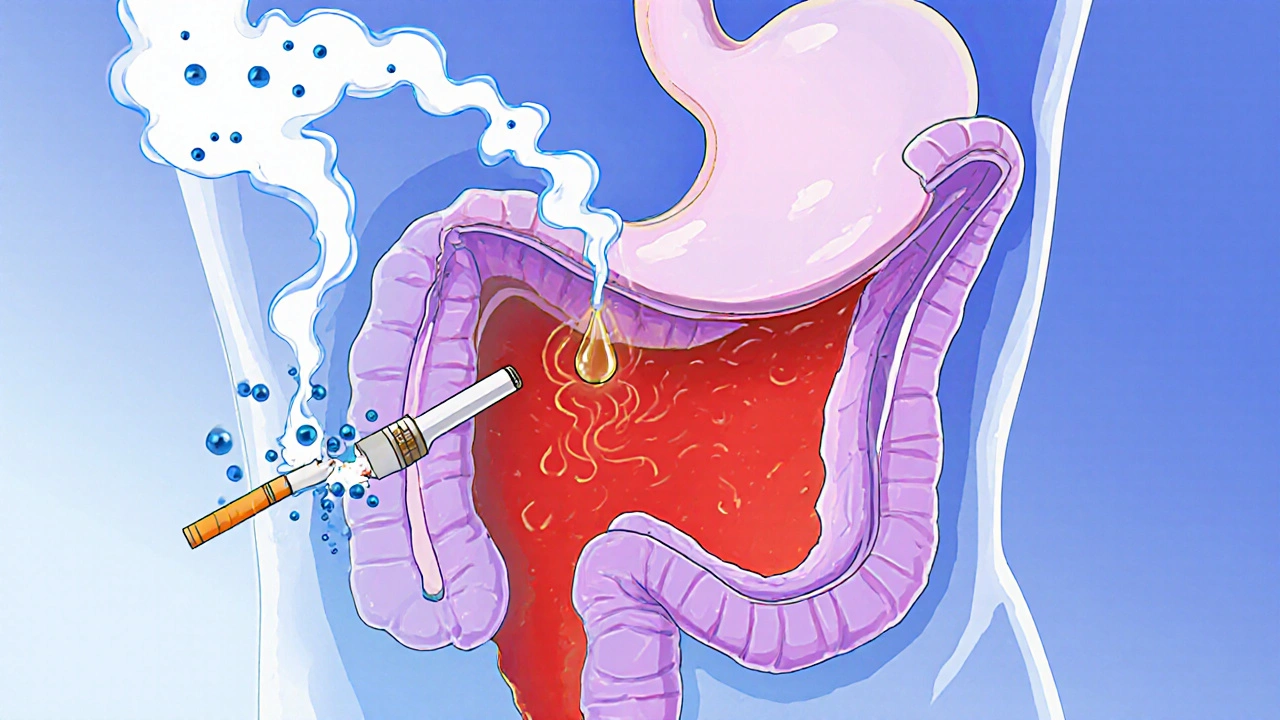
When you feel that burning sensation after a big meal, you’re probably dealing with acid indigestion - a common term for heartburn or gastro‑esophageal reflux disease (GERD). It happens when stomach acid slips back into the esophagus, irritating the lining and triggering that uncomfortable pain. Two everyday habits - lighting up a cigarette and raising a glass of wine or beer - can turn a mild twinge into a daily nightmare. Below we unpack why smoking and alcohol act like sabotage agents for your stomach, what symptoms to watch for, and how to protect yourself without giving up everything you love.
What exactly is acid indigestion?
Acid indigestion, or a condition where stomach acid repeatedly backs up into the esophagus, causing heartburn, sour taste, and sometimes chest pain, isn’t just a fleeting discomfort. Over time it can erode the esophageal lining, leading to inflammation (esophagitis), strictures, or even precancerous changes. The key player is the lower esophageal sphincter (LES) - a muscular ring that should stay tightly closed after food passes into the stomach. When the LES weakens or relaxes at the wrong moment, acid flows upward, and that’s when the pain starts.
How smoking interferes with the LES
Smoking isn’t just a lung problem; it messes with the entire digestive system. The nicotine in cigarettes triggers the release of adrenaline, which temporarily relaxes smooth muscles - including the LES. Studies from the National Institute of Health in 2023 showed that smokers have a 30% higher chance of LES relaxation after a meal compared to non‑smokers. In plain terms, every puff makes the LES more likely to ‘open the gate’ when it should stay shut.
- Reduced saliva production: Saliva neutralizes acid, but nicotine dries out the mouth, cutting off this natural buffer.
- Increased stomach acid: Nicotine stimulates gastric cells to pump out more acid, raising the pressure that pushes against the LES.
- Impaired healing: Smoking slows tissue repair, so any acid‑induced damage to the esophagus takes longer to mend.
Combine these effects and you get a perfect storm: a weaker gate, more acid behind it, and a slower recovery process.
Alcohol’s double‑edged strike
Alcohol behaves similarly but with a few extra tricks. First, it’s a direct irritant: even a small glass can weaken the LES within minutes. Second, alcohol relaxes the smooth muscle of the gastrointestinal tract, again lowering LES tone. Third, many alcoholic drinks are acidic or carbonated, adding extra acid load to the stomach. A 2022 meta‑analysis of 15 clinical trials found that moderate drinkers (one drink per day) were 22% more likely to report weekly heartburn than abstainers.
- Acid production boost: Alcohol stimulates gastrin, a hormone that tells the stomach to secrete more acid.
- Delayed gastric emptying: Alcohol slows the stomach’s ability to move food onward, keeping it longer in an acidic environment.
- Histamine release: Certain drinks, especially wine, cause histamine spikes that can inflame the esophageal lining.
When smoking and alcohol team up
If you both smoke and sip, the impact isn’t just additive - it’s multiplicative. The nicotine‑induced LES relaxation pairs with alcohol’s muscle‑relaxing effect, creating a near‑open gate. Moreover, both raise stomach acid, so the pressure pushing the acid upward skyrockets. A 2024 cohort study of 4,200 adults showed that smokers who drank socially were twice as likely to develop chronic GERD symptoms compared to those who only smoked or only drank.
In practical terms, you might notice:
- Heartburn attacks within 30 minutes of a night out.
- Morning soreness after a weekend binge.
- More frequent use of antacids, yet diminishing relief.
Symptoms that signal more than just a spice overload
Many people chalk up a burning chest to spicy food, but certain signs suggest smoking or alcohol are the hidden culprits:
- Burning that worsens when you’re lying down or after a cigarette.
- A sour or bitter taste that appears shortly after drinking.
- Hoarseness, chronic cough, or feeling of a lump in the throat - all linked to acid irritating the throat.
- Weight loss without trying - chronic reflux can affect appetite.
If any of these persist for more than a few weeks, it’s time to see a healthcare provider. Untreated GERD can lead to Barrett’s esophagus, a precancerous condition.
Quick fixes you can try tonight
Before you reach for the next cigarette or sip, try these low‑effort tweaks that can curb the burn:
- Delay the first drink: Give your LES 60-90 minutes after eating to settle before you start drinking.
- Choose low‑acid drinks: Clear spirits with water or low‑pH cocktails (like a gin‑tonic with a splash of cucumber) are gentler than wine or beer.
- Quit or cut back on smoking: Even reducing to a few cigarettes a day can improve LES function within weeks.
- Stay upright: Avoid lying down for at least two hours after meals or drinking.
- Chew gum: It stimulates saliva, which helps neutralize acid.
These aren’t cures, but they can buy you some relief while you work on longer‑term changes.
Long‑term lifestyle strategies
For lasting improvement, think of your digestive system as a team you need to train rather than a battlefield you can fight once and win.
- Quit smoking: The gold standard is complete cessation, but if that feels too steep, consider nicotine‑replacement patches or prescription aids. Within 1-2 months, LES pressure often returns to baseline.
- Moderate alcohol: The CDC defines moderate drinking as up to one drink per day for women and up to two for men. Staying under these limits can dramatically lower reflux episodes.
- Eat smaller, frequent meals: Large meals increase stomach distension, pushing acid upward. Aim for 4-6 modest portions.
- Identify trigger foods: Common culprits include citrus, tomato‑based sauces, chocolate, and fatty fried items. Keep a simple diary for two weeks and note when heartburn spikes.
- Maintain a healthy weight: Excess abdominal fat puts extra pressure on the stomach, encouraging reflux. A 5% weight loss can cut symptoms by up to 40%.
- Consider medications wisely: Over‑the‑counter antacids give quick relief, but proton‑pump inhibitors (PPIs) or H2 blockers are better for chronic cases. Always discuss with a doctor before long‑term use.
When to seek professional help
Occasional heartburn is normal, but you should schedule a medical appointment if you notice any of the following:
- Pain that lasts more than three weeks despite lifestyle changes.
- Difficulty swallowing or a sensation of food getting stuck.
- Unexplained weight loss or vomiting.
- Chest pain that mimics a heart attack (tightness, radiating to the arm or jaw).
Doctors may recommend an upper endoscopy, pH monitoring, or esophageal manometry to assess LES function and rule out more serious conditions.
Comparison: Smoking vs. Alcohol vs. Both on Acid Indigestion
| Factor | Mechanism | Acute Effect (within 1hr) | Chronic Effect (6+ months) | Risk Increase % |
|---|---|---|---|---|
| Smoking | Nicotine relaxes LES, reduces saliva, raises stomach acid | 30‑40% LES pressure drop | Higher incidence of GERD, slower esophageal healing | 30% |
| Alcohol | Direct LES relaxation, increased gastrin, acidic/ carbonated drinks | 20‑35% LES pressure drop, increased acid output | Elevated chronic reflux, potential esophagitis | 22% |
| Both | Combined muscle relaxation + acid surge + saliva loss | 60‑70% LES pressure drop, rapid symptom flare‑up | Nearly double GERD odds, higher Barrett’s risk | ≈50% |
These numbers illustrate why tackling both habits yields the biggest health payoff. Cutting out one alone helps, but addressing the pair is what truly reduces the fire.
Practical next steps
Pick the action that feels most doable right now and lock it in:
- Set a quit‑date for cigarettes and enlist a buddy or app for accountability.
- Swap your nightly wine for sparkling water with a splash of citrus - you still get the ritual without the acid surge.
- Start a simple reflux diary: note meals, drinks, smoking episodes, and symptom severity on a 1‑10 scale.
- Schedule a check‑up if symptoms persist after two weeks of these changes.
Small, consistent steps beat grand, unsustainable vows every time.
Frequently Asked Questions
Can I still have a glass of wine if I have acid indigestion?
Yes, but moderation is key. Limit yourself to one small glass (about 5oz) and pair it with food that’s low in acid and fat. Keep a gap of at least an hour after eating before you start drinking, and watch for any increase in heartburn.
How quickly does smoking affect the LES after a cigarette?
Nicotine starts acting within minutes, and LES pressure can drop by about a third within 15‑30 minutes. The effect may linger for up to two hours, especially if you chain cigarettes.
Are antacids enough if I smoke and drink?
Antacids neutralize existing acid but don’t fix the underlying LES weakness caused by nicotine or alcohol. For frequent symptoms, a doctor might suggest H2 blockers or proton‑pump inhibitors, alongside lifestyle changes.
What’s the best way to quit smoking if I’m worried about reflux?
Combine nicotine‑replacement therapy (patches or gum) with behavioral support. Many find that cravings lessen within a few weeks, and LES pressure usually rebounds to normal within 1‑2 months, cutting reflux episodes dramatically.
Is there a safe amount of alcohol for someone with GERD?
The safest approach is to stay within CDC’s moderate‑drinking guidelines - up to one drink per day for women and two for men - and choose low‑acid options. Even then, monitor how your body reacts and adjust accordingly.



lucy kindseth
October 4, 2025 AT 12:12Smoking and booze are like the dynamic duo of digestive disaster. Every puff of nicotine throws the lower esophageal sphincter into a lazy slump, making it easy for acid to escape. Meanwhile, alcohol acts as a chemical relaxant, further loosening the gate and cranking up stomach acid production. The result is a perfect storm where heartburn strikes faster and hangs around longer. Studies from the NIH in 2023 show smokers are thirty percent more likely to suffer LES relaxation after meals. A 2024 cohort of over four thousand adults found that the combination of smoking and drinking doubled the odds of chronic GERD. Even moderate drinking, just one glass a day, nudges the risk up by twenty-two percent compared to total abstinence. Heavy drinkers who push past ten drinks a week see their acid levels spike dramatically, overwhelming the stomach’s natural buffers. On the flip side, cutting back on cigarettes can restore LES pressure to baseline in as little as six weeks. Swapping wine for a low‑acid cocktail or sparkling water can shave off those late‑night heartburn episodes. Keeping a simple reflux diary helps you spot patterns you might otherwise miss. Small lifestyle tweaks-like waiting an hour after eating before drinking-can make a big difference. Chewing gum after meals boosts saliva, which naturally neutralizes acid. If symptoms persist, it’s wise to talk to a doctor about PPIs or H2 blockers as a longer‑term solution. Bottom line: quitting smoking and moderating alcohol are the most powerful tools you have to tame acid indigestion.
Earl Hutchins
October 5, 2025 AT 04:52Smoking relaxes the LES and alcohol adds more acid; cut both and you’ll feel the burn fade fast.
Tony Bayard
October 5, 2025 AT 21:32Picture this: you light up, take a sip, and within minutes your stomach is staging a rebellion, spewing acid like a dragon that’s had too much ale. The drama is real, and the only hero you need is a determined quit‑and‑cut plan.
Karen McCormack
October 6, 2025 AT 14:12In the grand tapestry of bodily alchemy, nicotine and ethanol are the mischievous sprites that untether the esophageal gate, allowing the acidic tide to breach the shores of comfort. Their synergy is nothing short of poetic chaos, a reminder that our choices echo in the chambers of our gut.
Nymia Jones
October 7, 2025 AT 06:52Let us not be fooled by the mainstream narrative that paints smoking and drinking as mere personal habits; they are, in fact, orchestrated tools of a shadowy elite seeking to undermine our health. The chemicals released not only erode the LES but also serve as conduits for deeper societal control. One must awaken to this reality and reject these insidious agents with unwavering resolve.
Jay Crowley
October 7, 2025 AT 23:32Cut the smoke and booze, feel better.
sharon rider
October 8, 2025 AT 16:12From a cultural standpoint, many societies have long recognized the link between hearty meals, spirits, and indigestion, often embedding modest drinking practices into rituals to avoid exactly these problems.
swapnil gedam
October 9, 2025 AT 08:52I’ve been tracking my own reflux for a few weeks, noting every cigarette and drink, and the patterns are unmistakable – the acid flare‑ups line up almost perfectly with my smoking breaks and post‑dinner beers. It’s a clear reminder that personal data can guide us better than generic advice.
Michael Vincenzi
October 10, 2025 AT 01:32Great tips, Lucy! I’ll start logging my drinks and try the gum trick tonight – fingers crossed it helps.
Courage Nguluvhe
October 10, 2025 AT 18:12From a pathophysiological perspective, ethanol acts as a pharmacologic smooth‑muscle relaxant, diminishing sphincteric tone, while nicotine up‑regulates gastrin secretion – a synergistic derangement of the gastro‑esophageal axis.
Oliver Bishop
October 11, 2025 AT 10:52As proud Americans, we know our freedom includes the right to a healthy gut, so let’s ditch the smoke and limit the booze for a stronger nation.
Alissa DeRouchie
October 12, 2025 AT 03:32Really? You think a glass of wine is the villain here? Everyone knows it’s just the stress of modern life, not the drink itself.
Emma Howard
October 12, 2025 AT 20:12Let’s power through this together! Cut back on the cigarettes, sip water instead of beer, and you’ll see the burning fade – you’ve got this!
dee gillette
October 13, 2025 AT 12:52While the article presents sound advice, it neglects to address the socioeconomic factors that limit many individuals’ ability to modify these habits.
Jasin P.
October 14, 2025 AT 05:32Oh sure, quit smoking and drinking, as if that’s a simple switch‑flip. Good luck navigating that maze while the healthcare system watches you drown.
Lily Đàn bà
October 14, 2025 AT 22:12Honestly, the drama of “acid indigestion” is just an excuse for people to keep their unhealthy habits; they’d rather blame the fire than face their own choices.
Joseph O'Sullivan
October 15, 2025 AT 14:52It’s funny how we treat the gut like a rebellious teenager – you feed it booze and smokes, then blame it for the tantrums. Maybe the real lesson is to respect the body’s boundaries.