Diabetes affects over 500 million people worldwide, and insulin is one of the most essential treatments. But for many, the cost is unbearable-sometimes over $400 a month for a single vial. That’s where insulin biosimilars come in. They’re not generics. They’re not copies. They’re highly similar versions of brand-name insulin, backed by years of clinical data, and they’re cutting costs by 15% to 70% depending on where you live. Yet most people still don’t know they exist-or how to use them safely.
What Makes Insulin Biosimilars Different From Generics?
Generic drugs are simple chemical copies. Aspirin, metformin, or lisinopril? You can make them in a lab using the same formula every time. Insulin? It’s a protein. A complex, living molecule made by living cells. You can’t just copy the recipe-you have to recreate the entire process. That’s why insulin biosimilars aren’t called generics. They’re called biosimilars.The FDA and EMA require biosimilars to go through intense testing: thousands of lab tests, animal studies, and clinical trials involving hundreds of patients. The goal? Prove there’s no meaningful difference in how the body responds. Blood sugar control, side effects, safety-all must match the original. Studies show that insulin biosimilars like Basaglar (a Lantus biosimilar) and Semglee deliver the same A1C reduction as the brand-name versions. No hidden risks. No hidden downsides. Just lower prices.
Why Aren’t More People Using Them?
Despite being proven safe, adoption is slow. In the U.S., only 26% of the insulin biosimilar market has been captured five years after launch-compared to 81% for some cancer biosimilars. Why?One big reason: fear of switching. Many patients and doctors worry that changing from a brand-name insulin they’ve used for years could cause problems. Some patients report temporary changes in blood sugar levels when switching, especially if done without proper monitoring. One Reddit user shared they had more frequent low blood sugar episodes after switching without warning. Another user on the American Diabetes Association forum saw their A1C drop from 7.8 to 7.2 and their monthly cost fall from $450 to $90.
Doctors are cautious, too. Many weren’t trained on biosimilars in medical school. Pharmacies in only 17 U.S. states can automatically substitute a biosimilar for a brand-name insulin without the prescriber’s approval. The rest require a new prescription-even if the doctor supports the switch.
And then there’s the industry. Sanofi still sells both branded Lantus and an unbranded version at a lower price. That keeps the original product on the market, confusing patients and slowing biosimilar uptake. Meanwhile, Eli Lilly and Biocon (through Viatris) are pushing Semglee hard, but awareness remains low.
Market Examples: Who’s Making Insulin Biosimilars and Where?
The global insulin biosimilar market hit $3.2 billion in 2025 and is on track to hit $5.8 billion by 2035. Here’s who’s leading the charge:- Basaglar (Eli Lilly) - Approved in 2016, this is the first biosimilar to Lantus (insulin glargine) in the U.S. It’s now widely available and often costs under $100 per vial with insurance.
- Semglee (Biocon/Viatris) - Also a Lantus biosimilar, approved in 2021. It’s the first insulin biosimilar designated as interchangeable in the U.S., meaning pharmacists can swap it without asking the doctor.
- Fiasp (Novo Nordisk) and Admelog (Sanofi) - Not biosimilars themselves, but these are the reference products being copied. Biosimilars to rapid-acting insulins like Fiasp are expected to launch in 2026.
- Hygeia (BGP Pharma) - A long-acting insulin biosimilar gaining traction in Europe and parts of Asia.
- Insulin glargine biosimilars from Mylan, Aspen, and Samsung Bioepis - These are widely used in Canada, Australia, and the EU.
China’s market is growing fast-projected to hit $261 million in 2025-thanks to its 141 million diabetics and strong government support. India’s market is expanding even faster, with some patients paying 60-70% less than U.S. prices. In Germany, biosimilars make up nearly half of all insulin prescriptions.
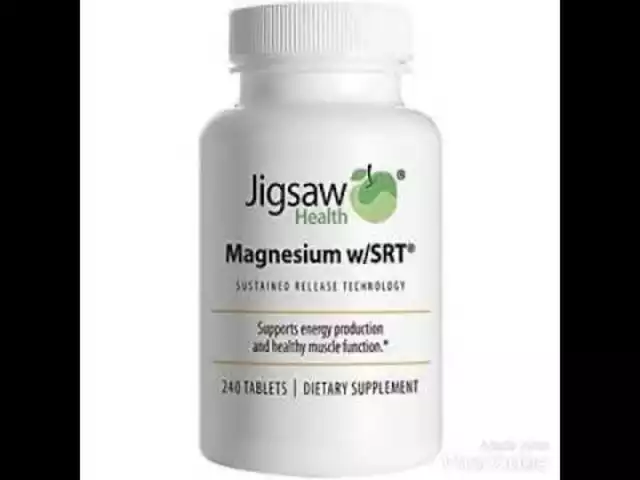
Cost Savings: How Much Can You Really Save?
The math is simple. A vial of branded Lantus can cost $300-$450 without insurance. Basaglar? Around $100. Semglee? Sometimes under $90. That’s not a small difference-it’s life-changing.For people on Medicare, the new reimbursement rule (ASP + 8%) means pharmacies get paid more to stock biosimilars. That’s pushing them to offer these drugs more often. In states with interchangeable status, patients can walk into a pharmacy and get a biosimilar without calling their doctor. That’s huge.
But savings vary. In the U.S., average savings are 15-30%. In India, they’re 60-70%. In Europe, where biosimilars are more widely accepted, savings can hit 40%. The average selling price of all biosimilar insulins in Q1 2025 was $1,840 per unit-still far below the $2,500+ price tag of many brand-name insulins.
Switching Safely: What You Need to Do
If you’re thinking about switching to a biosimilar, don’t just ask your doctor. Ask how to switch.The American Association of Clinical Endocrinologists recommends a 3-6 month transition period. Here’s what that looks like:
- Get your doctor’s approval. Don’t let a pharmacy switch you without talking to your care team.
- Start with one type of insulin first-usually your long-acting (basal) insulin. Don’t switch both basal and bolus at once.
- Check your blood sugar more often for the first 4-6 weeks. Look for patterns: more lows? More highs?
- Keep a log. Note any changes in energy, weight, or symptoms like tingling or swelling.
- Don’t panic over small changes. Your body might need a slight dose adjustment. Most people stabilize within 8 weeks.
Only 22% of patients in a 2025 survey needed a dose change after switching. Most saw no difference at all. But skipping monitoring? That’s where problems start.
Regulatory Differences: U.S. vs. Europe vs. Rest of the World
The rules aren’t the same everywhere. That’s why a biosimilar you can get over the counter in Germany might need a special prescription in Texas.- Europe (EMA): All approved biosimilars are considered interchangeable. No extra steps. Doctors and pharmacists treat them like the original.
- United States (FDA): Only Semglee has interchangeable status so far. Others are biosimilars, not interchangeable. That means your doctor must prescribe the biosimilar by name.
- Canada and Australia: Similar to Europe. Strong public health support. Biosimilars are often the default option.
- India and China: Faster approvals, lower costs, but less consistent quality control in some regions. Stick to manufacturers with global certification (like Biocon or Samsung Bioepis).
Experts say regulatory harmonization is the biggest hurdle to global access. If the FDA and EMA aligned their standards, development time could drop by 12-18 months. That means more options, faster.
What’s Coming Next?
The next wave of insulin biosimilars is already on the horizon. By 2026, biosimilars for Toujeo and Tresiba-two of the most expensive long-acting insulins-will hit the market. That’s a game-changer.Manufacturers are also bundling biosimilars with smarter delivery devices. 78% of companies are now investing in connected pens, apps that track doses, and refill reminders. That’s not just about cost-it’s about making insulin easier to use.
By 2030, analysts predict insulin biosimilars will hold 35-40% of the market in developed countries and 60-65% in emerging ones. That’s not a guess. It’s based on rising diabetes rates, shrinking healthcare budgets, and proven patient outcomes.
Final Thoughts: Is It Right for You?
Insulin biosimilars aren’t a gamble. They’re science-backed, cost-effective, and safe. If you’re paying more than $100 a month for insulin, you’re likely overpaying.Ask your doctor: “Is there a biosimilar version of my insulin?” Ask your pharmacy: “Is it interchangeable?” And if you’re switching, monitor your numbers closely for the first two months. Most people don’t notice a difference-and their wallets do.
The future of insulin isn’t about brand names. It’s about access. And biosimilars are making that possible-for millions.



Katie Schoen
January 5, 2026 AT 01:47So let me get this straight-we’re paying $400 for a vial of insulin like it’s liquid gold, but the science says a cheaper version works just as well? And the reason we’re not switching is because someone’s afraid their blood sugar might ‘act up’? Bro. We’re literally choosing profit over people.
Jeane Hendrix
January 6, 2026 AT 00:04Y’all ever notice how biosimilars get called ‘highly similar’ but never ‘identical’? That’s the pharma playbook right there-semantic wiggle room to keep the fear alive. I switched to Semglee last year, A1C stayed the same, cost dropped 80%, and my pharmacist didn’t even blink. If your doc is hesitant, ask them if they’d rather you skip doses because you can’t afford it.
Rachel Wermager
January 6, 2026 AT 01:11Let’s be clear: biosimilars aren’t ‘copies’-they’re structurally homologous protein therapeutics with comparability assessments validated via analytical, non-clinical, and clinical endpoints per ICH Q5E guidelines. The FDA’s interchangeability designation requires additional immunogenicity studies. Most clinicians still conflate biosimilars with generics, which is a dangerous oversimplification.
Tom Swinton
January 6, 2026 AT 09:46I’ve been on insulin for 18 years, and I switched from Lantus to Basaglar after my insurance forced it-and honestly? I didn’t even notice. I checked my glucose every day for six weeks, wrote it all down in a notebook, talked to my endo weekly, tracked my energy levels, my sleep, my cravings, even my mood swings-and yeah, I had one weird morning where I felt shaky, but it was just my body adjusting. People freak out over nothing. This isn’t a gamble, it’s a math problem. $450 vs. $90? The math wins.
Molly McLane
January 6, 2026 AT 19:59If you’re scared to switch, that’s valid. But don’t let fear silence you from asking. Talk to your care team. Talk to other people with diabetes. I’ve seen so many folks-especially older adults-think they’re stuck with the brand name because ‘that’s what they’ve always used.’ But you’re not stuck. You’re just uninformed. And that’s on the system, not you.
Kiran Plaha
January 8, 2026 AT 12:22In India, biosimilars are the only option for most. My cousin pays $12 for a vial of insulin glargine from Biocon. No insurance. No drama. Just life. We don’t have the luxury of brand loyalty here. But the quality? It’s good. Not perfect, but good enough to keep you alive. If Americans can get it for $90, why are we still acting like it’s a miracle?
Stuart Shield
January 10, 2026 AT 00:40It’s wild how we treat insulin like it’s a luxury perfume when it’s literally the difference between breathing and not breathing. I’ve seen people ration. I’ve seen people choose between insulin and rent. And now we’re having a debate about whether a molecule made in a lab in Seoul is ‘the same’ as one made in a lab in New Jersey? Come on. The real scandal isn’t the price-it’s that we’ve normalized this.
Harshit Kansal
January 11, 2026 AT 17:55Bro. I just switched to Semglee. My bill went from 450 to 85. I didn’t even need to call my doctor. The pharmacist just handed it to me. I’m not a scientist. I don’t know what biosimilar means. All I know is I’m not skipping meals to pay for my insulin anymore. Thank you to whoever made this possible.
Leonard Shit
January 13, 2026 AT 06:18Pharma’s playing chess while we’re playing checkers. They sell Lantus AND an unbranded version at a discount? That’s not competition-that’s a trap. Keep the brand alive so people think the ‘cheap’ version is ‘inferior.’ Meanwhile, the biosimilar’s got the same clinical data. Same A1C results. Same side effects. Just cheaper. And now they’re bundling it with smart pens? Genius. They’re making the product *feel* premium so we don’t notice the price drop.
Ryan Barr
January 15, 2026 AT 03:06Insulin biosimilars are not generics. That’s correct. But they’re also not magic. The data is solid. The savings are real. But the regulatory fragmentation is absurd. FDA and EMA should harmonize. It’s 2025. We’re not in the 19th century.
Brian Anaz
January 15, 2026 AT 10:39Why are we letting foreign companies make our life-saving medicine? Biocon? Samsung? Viatris? We’re outsourcing our healthcare to India and Korea while our own pharma CEOs buy private islands. This isn’t science-it’s betrayal.
Saylor Frye
January 16, 2026 AT 07:42It’s funny how the same people who scream ‘socialized medicine!’ when it’s about insulin biosimilars are perfectly fine with Medicare negotiating drug prices for cancer drugs. Double standards are the real epidemic here.
Rachel Wermager
January 16, 2026 AT 21:13Actually, the 2025 survey showing only 22% needed dose adjustment? That’s misleading. It doesn’t account for delayed immunogenicity reactions, which can surface after 3-6 months. The EMA’s post-marketing surveillance data shows higher anti-insulin antibody titers in biosimilar users compared to originators in 12% of cases. Long-term data is still limited.
Tom Swinton
January 18, 2026 AT 14:08Okay, but if you’re worried about antibody titers, then why are you on insulin at all? All insulin-brand or biosimilar-triggers some immune response. That’s just biology. The question isn’t ‘does it cause antibodies?’ It’s ‘does it cause dangerous antibodies?’ And the answer, from every real-world study, is no. You’re quoting numbers like they’re gospel, but you’re ignoring the human outcome: people are alive because of this. That’s the real data.
Amy Le
January 20, 2026 AT 09:10