Over 32 million Americans live with Osteoarthritis (a degenerative joint disease caused by mechanical wear and tear on joints). It’s the most common type of arthritis, but many people confuse it with rheumatoid arthritis. Getting the diagnosis wrong can lead to serious consequences. Let’s break down the real differences.
What is Osteoarthritis?
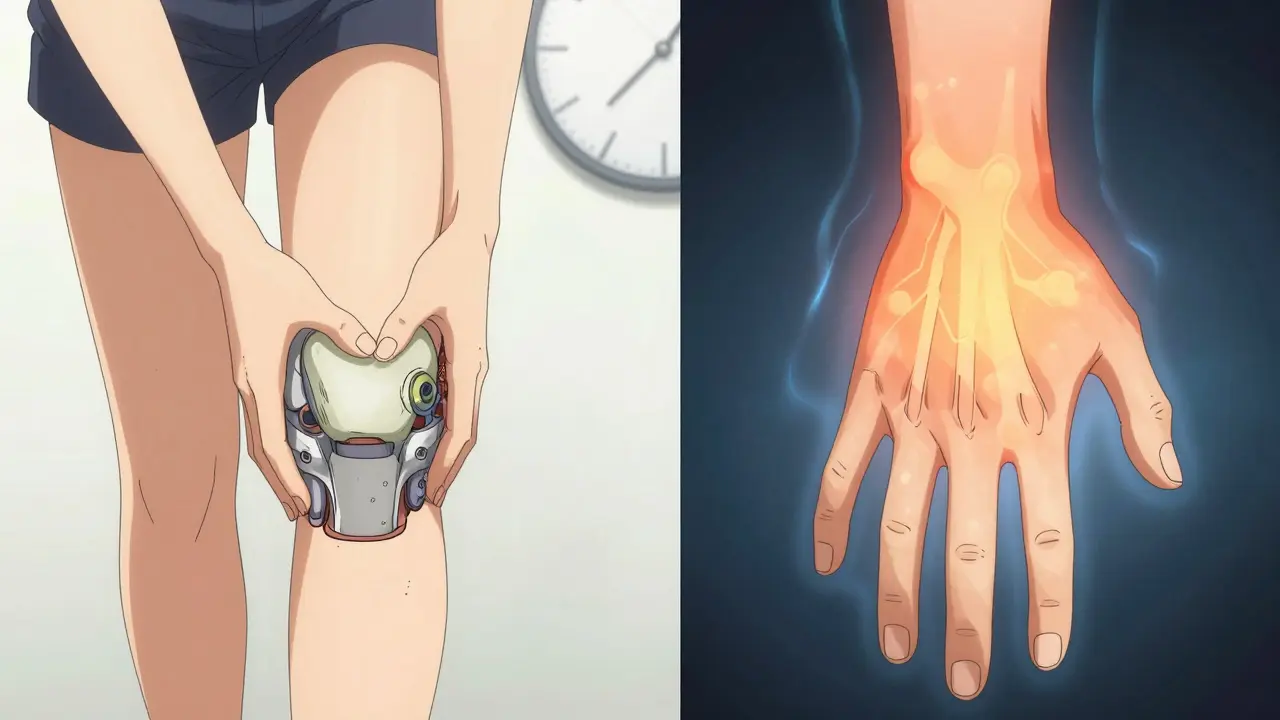
Osteoarthritis (OA) happens when the cartilage cushioning your joints wears down over time. This causes bones to rub together, leading to pain, stiffness, and swelling. It’s often called "wear and tear" arthritis because it’s linked to aging, joint injuries, or repetitive stress. Common in weight-bearing joints like knees, hips, and spine, but it can also affect hands-especially the joints closest to the fingertips (DIP joints) and middle finger joints (PIP joints).
Unlike other types, OA usually affects one side of the body more than the other. For example, your right knee might hurt more than your left. Morning stiffness typically lasts less than 30 minutes and improves with movement. Pain tends to worsen during activity and improve with rest. Obesity is a major risk factor-each extra pound adds four pounds of pressure on your knees. Losing just 5kg can reduce knee OA pain by half.
What is Rheumatoid Arthritis?
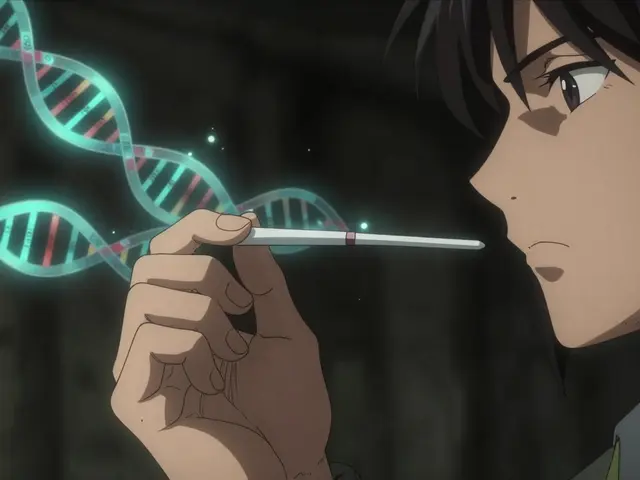
Rheumatoid arthritis (RA) is an autoimmune disorder where your immune system mistakenly attacks healthy joint tissue. This causes inflammation in the synovial membrane lining the joints, leading to pain, swelling, and eventually joint damage. RA isn’t just about joints-it’s a systemic condition that can affect the lungs, heart, and eyes.
Symptoms often develop quickly over weeks or months. Morning stiffness usually lasts longer than an hour and may not improve until later in the day. Joint pain is symmetrical-both wrists, both knees, etc. RA commonly targets the knuckles (MCP joints), wrists, and PIP joints but spares the DIP joints near the fingertips. Blood tests for rheumatoid factor (RF) and anti-CCP antibodies help confirm diagnosis. Without early treatment, RA can cause permanent joint damage within months.
Other Types of Arthritis
While OA and RA make up most cases, there are over 100 types of arthritis. Psoriatic arthritis often occurs with psoriasis skin disease and affects joints and tendons. Gout results from uric acid crystals building up in joints, causing sudden severe pain, usually in the big toe. Lupus is another autoimmune condition that can cause joint pain along with skin rashes and organ involvement. Each type requires different management strategies.

Key Differences Between OA and RA
| Aspect | Osteoarthritis | Rheumatoid Arthritis |
|---|---|---|
| Primary Cause | Joint wear and tear over time | Autoimmune attack on joint lining |
| Symptom Onset | Gradual, over years | Rapid, weeks to months |
| Joint Symmetry | Often asymmetrical | Always symmetrical |
| Morning Stiffness | Less than 30 minutes | Over one hour |
| Systemic Symptoms | None | Yes (fatigue, fever, weight loss) |
| Commonly Affected Joints | Knees, hips, DIP joints in hands | MCP joints, wrists, PIP joints |
| Diagnostic Tests | X-rays (joint space narrowing) | Blood tests (RF, anti-CCP antibodies) |
| Primary Treatments | NSAIDs, weight management, physical therapy | DMARDs, biologics |
How Doctors Diagnose Each Type
OA diagnosis typically starts with a physical exam and X-rays showing joint space narrowing or bone spurs. Blood tests aren’t usually needed since there’s no specific blood marker for OA. RA diagnosis is more complex. Doctors look for symmetrical joint swelling and order blood tests for rheumatoid factor (RF) and anti-CCP antibodies. Ultrasound or MRI may also detect early inflammation in the synovium. A key difference: OA shows joint damage on X-rays, while RA shows inflammation in blood tests and imaging.
Treatment Differences
OA management focuses on reducing joint stress. Weight loss is critical-5kg lost can cut knee pain by half. Physical therapy strengthens muscles around joints, while NSAIDs like ibuprofen help manage pain. In severe cases, joint replacement surgery is common. Over 90% of US joint replacements are for OA.
RA treatment requires aggressive early action. Disease-modifying antirheumatic drugs (DMARDs) like methotrexate suppress the immune system to prevent joint damage. Biologic drugs target specific immune pathways. Starting treatment within 3-6 months of symptoms is crucial for better outcomes. Delaying RA treatment can lead to permanent disability.
Why Getting the Right Diagnosis Matters
Mistaking RA for OA could mean missing critical immune-suppressing treatment. Without DMARDs, RA can destroy joints within months. Conversely, using strong immunosuppressants for OA would be unnecessary and risky. For example, a patient with hand pain might assume it’s OA, but if it’s RA, waiting to treat it could lead to permanent deformity. Doctors rely on symptom patterns, blood tests, and imaging to distinguish between them-so accurate diagnosis is everything.
Can you have both osteoarthritis and rheumatoid arthritis?
Yes. It’s possible to have both conditions, especially as you age. Osteoarthritis often affects older adults, while RA can occur at any age. Someone with RA might develop OA in the same joints due to previous damage. Doctors need to manage both separately-RA requires immune-suppressing drugs, while OA focuses on joint protection and pain relief.
Is arthritis only a problem for older people?
No. While osteoarthritis is more common in older adults, rheumatoid arthritis can start as early as your 20s or 30s. Juvenile idiopathic arthritis affects children under 16. Even gout and psoriatic arthritis can occur in younger people. Age isn’t a barrier-anyone can develop arthritis.
Does exercise help with arthritis?
Yes, but the type matters. For OA, low-impact exercises like swimming or walking strengthen muscles without stressing joints. For RA, gentle range-of-motion exercises help maintain flexibility during flare-ups. High-impact activities like running may worsen symptoms. Always consult a physical therapist to design a safe routine.
Can diet affect arthritis symptoms?
For OA, maintaining a healthy weight reduces joint stress. Some evidence suggests anti-inflammatory diets (rich in omega-3s, fruits, vegetables) may help RA symptoms. Avoiding processed foods and sugar can reduce inflammation. However, no single diet cures arthritis-work with a dietitian for personalized advice.
What’s the difference between morning stiffness in OA vs RA?
OA stiffness usually lasts less than 30 minutes and eases quickly with movement. RA stiffness often lasts over an hour and may persist throughout the day. This is because RA involves active inflammation, while OA stiffness is due to joint inactivity without systemic inflammation.

Dina Santorelli
February 6, 2026 AT 01:04Been living with OA for over a decade. The article says it's 'wear and tear' but that's just a surface-level explanation.
The real issue is chronic inflammation from processed foods.
I've seen my joints get worse when I eat fast food.
And RA isn't just joints-it affects your whole body.
The medical system ignores this.
They're all in bed with Big Pharma.
Drugs are not the solution.
Natural remedies like turmeric work better.
But they don't tell you that.
This is why people suffer.
The government and pharma are hiding the truth.
I'm tired of this.
Phoebe Norman
February 6, 2026 AT 10:23OA degenerative joint disease
RA autoimmune
key difference mechanical vs immune
Article misses systemic impact RA
Should emphasize DMARDs urgency
Early intervention prevents permanent damage
X-rays show OA joint space narrowing
Blood tests for RA RF anti-CCP
Simple
Albert Lua
February 7, 2026 AT 05:17Hey everyone! I'm from the US but have friends in Japan who use traditional medicine for arthritis.
Acupuncture and herbal remedies really help with OA pain.
For RA, they use similar approaches but focus on immune balance.
It's cool how different cultures handle this.
We should share these methods globally.
Arthritis affects all of us, so let's learn from each other!
Katharine Meiler
February 8, 2026 AT 12:01As a rheumatologist, I can confirm that RA diagnosis requires anti-CCP antibodies.
OA is confirmed via X-ray joint space narrowing.
The article correctly states this but misses the importance of early RA intervention.
Delaying treatment causes irreversible damage.
Must emphasize that.
Also, NSAIDs for OA can lead to GI issues-consider COX-2 inhibitors.
For RA, DMARDs are non-negotiable.
This is critical for patient outcomes.
Danielle Vila
February 8, 2026 AT 20:18This article is a cover-up.
Big Pharma and governments are hiding the truth about 5G causing arthritis.
They want you to take drugs so you stay dependent.
The real solution is avoiding Wi-Fi and eating raw garlic.
Trust me, I've done my research.
This is why people are getting sicker.
They're all part of the system.
Thorben Westerhuys
February 10, 2026 AT 10:45Oh my gosh! This is so important!
Wait, did you know that RA can affect the heart? Yes! It's systemic!
So many people don't realize that.
I had RA and it affected my lungs too.
The article should mention that more.
Also, morning stiffness-over an hour for RA, yes!
But the article doesn't say enough about how it's not just joints.
So important!
Also, the 5G conspiracy is nonsense.
It's all about autoimmune triggers like stress and infections.
Please stop spreading misinformation!
Laissa Peixoto
February 11, 2026 AT 03:02Arthritis is not just a physical condition-it's a reflection of our relationship with our bodies.
OA is the body's way of telling us we've been too hard on it.
RA is an internal conflict.
The real issue is how society treats chronic pain.
We need more compassion, not just medical solutions.
It's about understanding the whole person.
Lana Younis
February 12, 2026 AT 18:14Hey, this is a good point! 😊
I agree that arthritis is more than just physical.
In some cultures, like in India, they use yoga and Ayurveda for joint health.
But the article doesn't mention that.
Also, stress plays a big role.
Maybe we should talk more about mental health in arthritis care.
Typos everywhere but still useful!
one hamzah
February 14, 2026 AT 03:52Great article! 🌟 OA and RA are so different but both need attention.
I've seen in India how yoga helps OA symptoms.
For RA, early treatment is key.
Let's spread awareness! 💯 #ArthritisAwareness
Matthew Morales
February 16, 2026 AT 02:09This is super helpful! 😊
I had OA in my knees and weight loss really helped.
Lost 15 lbs and my pain dropped.
But the article should mention that physical therapy is crucial too.
Also, NSAIDs can cause stomach issues-maybe add a note about that.
Typos are everywhere but still useful!
Diana Phe
February 16, 2026 AT 08:55This article is a joke.
The real cause of arthritis is foreign chemicals in our food.
America needs to stop importing processed foods.
RA is just a symptom of the government's plan to control us.
We need to go back to natural foods.
Trust me, I've done my research.