Arthritis isn't just one condition-it's over 100 different arthritis types affecting joints. But two types dominate: osteoarthritis (OA) and rheumatoid arthritis (RA). They look similar but have totally different causes and treatments. Getting them mixed up can lead to serious health risks. Let's break down what makes them unique.
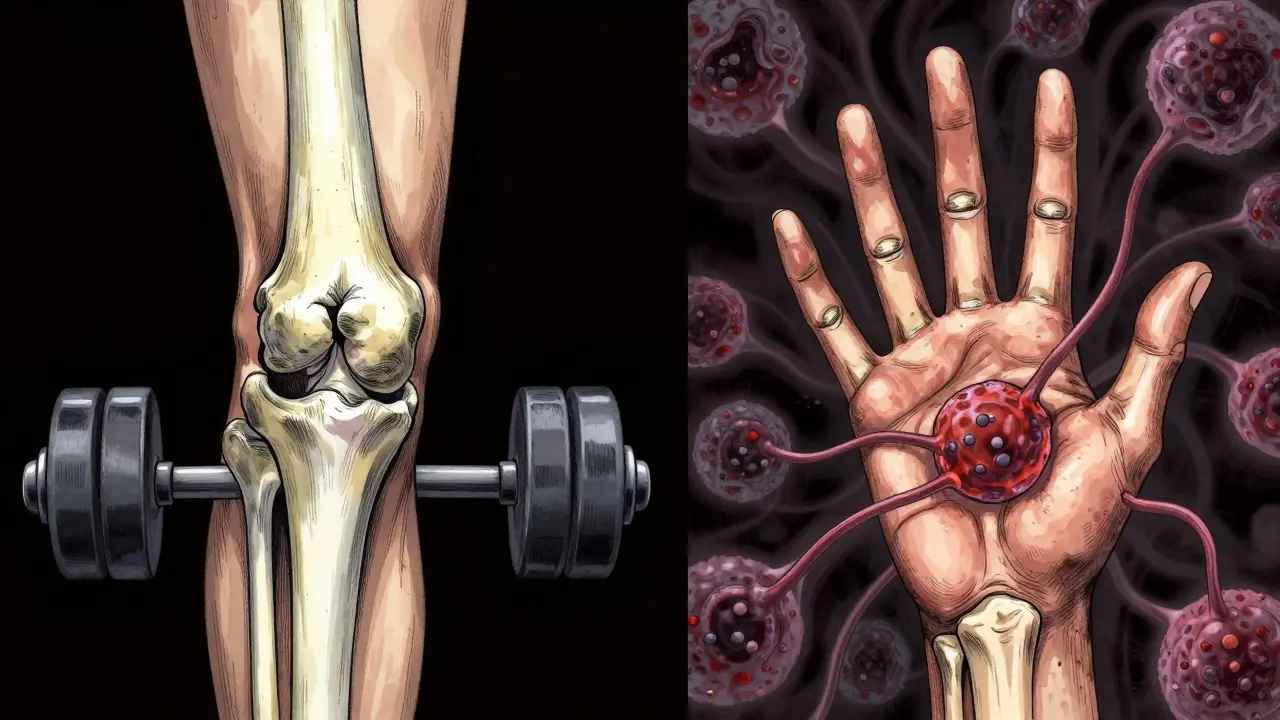
What is Osteoarthritis?
Osteoarthritis is a degenerative joint condition caused by mechanical wear and tear. It affects 32.5 million American adults, making it the most common arthritis type. Cartilage breaks down over time, causing bones to rub together. This leads to pain, swelling, and stiffness. Unlike other forms, OA usually hits weight-bearing joints first: knees, hips, spine, and hands-especially the joints closest to fingertips. Symptoms develop slowly. Pain worsens with activity but improves with rest. Morning stiffness typically lasts under 30 minutes. X-rays show joint space narrowing and bone spurs. Treatment focuses on managing pain and slowing progression. Weight loss is crucial-a 5kg reduction cuts knee OA pain by 50%. Physical therapy, NSAIDs like ibuprofen, and joint injections help. Severe cases may need surgery like joint replacement.
What is Rheumatoid Arthritis?
Rheumatoid Arthritis is an autoimmune disorder where the immune system attacks healthy joint tissue. It affects about 1.3 million Americans. RA symptoms develop faster than OA-over weeks or months. They include symmetrical joint pain (both wrists or knees at once), prolonged morning stiffness over an hour, fatigue, low fevers, and weight loss. Unlike OA, RA often affects smaller joints first: wrists, knuckles, and the base of fingers. Blood tests for rheumatoid factor (RF) and anti-cyclic citrullinated peptide (anti-CCP) antibodies confirm diagnosis. Untreated, RA can destroy joints in months. Treatment requires aggressive drugs called disease-modifying antirheumatic drugs (DMARDs). Methotrexate is the first-line option. Biologics like TNF inhibitors or newer JAK inhibitors (e.g., tofacitinib) target specific immune pathways. Early treatment within 3-6 months of symptoms is critical to prevent permanent damage.
Other Arthritis Types
While OA and RA are most common, other types exist. Gout results from uric acid crystal buildup, causing sudden, severe pain in the big toe. Psoriatic arthritis links to skin psoriasis and affects nails and joints. Each type has unique triggers and treatments. For example, gout responds to uric acid-lowering drugs, while psoriatic arthritis often needs biologics similar to RA. These conditions share joint pain but have distinct causes and management strategies.

Key Differences Table
| Aspect | Osteoarthritis | Rheumatoid Arthritis |
|---|---|---|
| Primary Cause | Wear and tear on joint cartilage | Autoimmune attack on joint lining |
| Symptoms | Asymmetric pain, worse with use, stiffness under 30 minutes | Symmetrical swelling, prolonged morning stiffness over an hour, fatigue |
| Diagnosis | X-rays showing joint space loss and bone spurs | Blood tests for rheumatoid factor and anti-CCP antibodies |
| Treatment | NSAIDs, weight management, joint replacement | DMARDs, biologics, early aggressive intervention |
| Systemic Impact | Limited to affected joints | Affects lungs, heart, eyes, and other organs |
Why Accurate Diagnosis Matters
Misdiagnosing OA as RA-or vice versa-can have serious consequences. OA treatment with painkillers won't stop RA's autoimmune damage. Delayed RA treatment leads to irreversible joint deformities. Conversely, using strong immunosuppressants for OA risks unnecessary side effects. Doctors use a mix of symptoms, blood tests, and imaging to differentiate them. For instance, OA typically shows asymmetric joint involvement and bone spurs on X-rays, while RA shows symmetrical swelling and positive RF/anti-CCP tests. A 2023 study in the Journal of Rheumatology found 20% of early arthritis cases were misdiagnosed, leading to worsened outcomes. This highlights why seeing a rheumatologist for unclear joint pain is critical.

Current Research and Treatment Advances
New tools are improving arthritis care. Ultrasound and MRI detect early joint damage before X-rays show changes. For RA, JAK inhibitors like tofacitinib offer alternatives when biologics fail. In OA, platelet-rich plasma (PRP) injections are being studied, though evidence is still mixed. Lifestyle changes remain key-quitting smoking cuts RA risk by 30%, and maintaining a healthy BMI slows OA progression. A 2024 clinical trial showed that combining weight loss with exercise reduced knee OA pain by 60% in obese patients. Meanwhile, new biologic drugs for RA are achieving remission in 40% of patients within one year.
Frequently Asked Questions
Can you have both OA and RA?
Yes, though it's rare. OA is wear-and-tear damage, while RA is autoimmune. Some people develop both, especially older adults with joint injuries. A 2022 study in Arthritis & Rheumatology found 8% of RA patients also had OA in the same joints. Managing both requires tailored treatment plans.
How do doctors diagnose RA?
Diagnosis combines blood tests, physical exams, and imaging. Blood tests check for rheumatoid factor (RF) and anti-CCP antibodies. X-rays or ultrasound look for joint damage. Symptoms like symmetrical swelling and morning stiffness over an hour help confirm. Early diagnosis within 3 months of symptoms improves outcomes significantly.
Is RA curable?
Not yet, but modern treatments can put it into remission. About 30-50% of RA patients achieve remission with early, aggressive therapy using DMARDs and biologics. Remission means no active inflammation, though ongoing treatment is usually needed to maintain it.
Can OA be prevented?
While aging is a factor, lifestyle changes reduce risk. Maintaining a healthy weight (BMI below 25) lowers knee OA risk by 50%. Avoiding joint injuries and staying active with low-impact exercises like swimming also helps. A 2023 study showed that regular physical activity delayed OA onset by 5 years in high-risk groups.
What's the difference between joint pain from OA and RA?
OA pain worsens with activity and improves with rest. Morning stiffness is brief (under 30 minutes). RA pain is constant, with prolonged morning stiffness (over an hour), fatigue, and systemic symptoms like fever. RA also affects joints symmetrically (both sides), while OA often starts on one side.


Dina Santorelli
February 4, 2026 AT 16:13OA isn't just mechanical wear. It's a complex systemic issue. Many studies show inflammation plays a role even in OA. The article misses that.
Phoebe Norman
February 4, 2026 AT 18:43OA involves cytokine mediated inflammation too Synovitis is part of it The articles wear and tear is outdated RA is autoimmune but OA has inflammatory components
Albert Lua
February 5, 2026 AT 19:58In many cultures, OA is treated with traditional remedies like turmeric and yoga. RA requires DMARDs. Understanding the difference saves lives.
Katharine Meiler
February 6, 2026 AT 13:26DMARDs are critical for RA management. Early intervention within 3 months significantly reduces joint damage. This is well-documented in rheumatology literature.
Danielle Vila
February 6, 2026 AT 14:15Big Pharma is hiding the truth about arthritis. They want you to think it's OA vs RA. It's actually all about fluoride in water. Look it up.
Thorben Westerhuys
February 8, 2026 AT 03:32This is why I distrust doctors! They're in on it. I read about fluoride on forums. It's everywhere! They're poisoning us to sell drugs.
Laissa Peixoto
February 9, 2026 AT 22:16Arthritis isn't just physical-it's emotional. The fear of losing mobility changes lives. Understanding the difference helps people cope.
Lana Younis
February 11, 2026 AT 21:04so true. the mental toll is real. i have a friend with RA and she's always stressed about her joints. but knowing it's autoimmune helps her get the right treatment. keep sharing this info! i've seen how much easier life is with proper care. it's not just about the joints; it's about being able to work, take care of kids, live normally. the difference between OA and RA is huge. OA is gradual, RA is sudden. OA pain gets worse with activity, RA pain is constant. OA doesn't affect organs, RA can. i read a study where early DMARDs prevented disability. it's not just about meds; lifestyle changes help too. exercise, diet, stress management. i'm so glad this article explains it all clearly. it's hard to find accurate info online. so many people get misdiagnosed. this is exactly what we need. more awareness, more education. thank you for breaking it down.
one hamzah
February 12, 2026 AT 09:29OA and RA are fundamentally different. One is mechanical, the other autoimmune.
Matthew Morales
February 14, 2026 AT 03:34OA is wear and tear. RA is autoimmune. They're not the same. 😊
Diana Phe
February 14, 2026 AT 16:19This is why we need American-made drugs. Foreign companies are pushing fake arthritis theories. The US is leading in research.
Carl Crista
February 16, 2026 AT 03:28US leads. China is behind. They don't know. Only US has real science. Other countries are wrong.
Andre Shaw
February 16, 2026 AT 03:49OA is actually RA. They're the same. The whole medical field is wrong. I've been researching for years. It's all autoimmune.
Dr. Sara Harowitz
February 16, 2026 AT 20:48As a doctor, I must say this is dangerously incorrect. OA and RA are distinct. Misinformation like this is why patients suffer. Please educate yourself.
Joyce cuypers
February 17, 2026 AT 19:34i agree with dr. harowitz. its important to get the right diagnosis. but we should also be compassionate. people with arthritis face so much. lets support each other. <3